Procedure 80 Corrective Osteotomy of Malunited Distal Radius Fractures
Indications
 Deformity by itself may or may not be symptomatic. A decision for surgery should be based on functional impairment, pain, loss of motion, and limitation of grip strength.
Deformity by itself may or may not be symptomatic. A decision for surgery should be based on functional impairment, pain, loss of motion, and limitation of grip strength.
 Alteration of radiocarpal alignment will affect normal carpal kinematics and changes in the vectors of the extensor and flexor tendons (Fig. 80-1).
Alteration of radiocarpal alignment will affect normal carpal kinematics and changes in the vectors of the extensor and flexor tendons (Fig. 80-1).
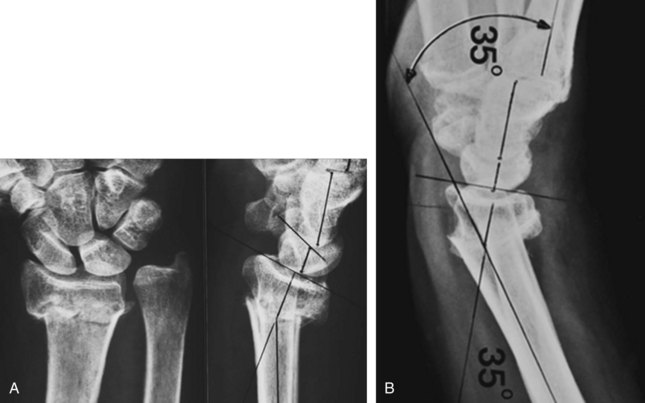
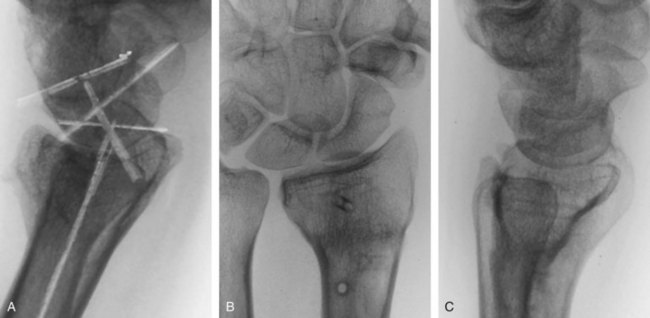
 Dorsally malunited fracture can result in a midcarpal instability (Figs. 80-2 and 80-3).
Dorsally malunited fracture can result in a midcarpal instability (Figs. 80-2 and 80-3).
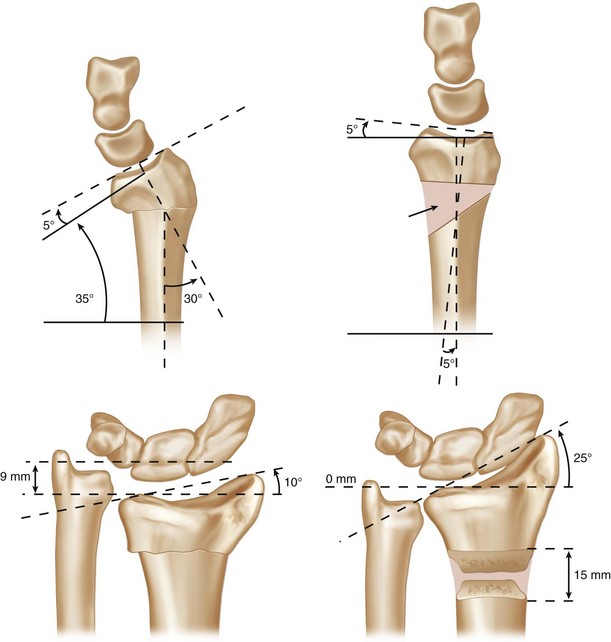
 Although there is no fixed radiographic criteria for correction of deformity, the lower limits of deformity at which symptoms are likely to be present include radial deviation of 20 to 30 degrees, sagittal tilt of 10 to 20 degrees dorsally, and radial shortening of 0 to 2 mm. Articular incongruity greater than 2 to 3 mm may also require osteotomy.
Although there is no fixed radiographic criteria for correction of deformity, the lower limits of deformity at which symptoms are likely to be present include radial deviation of 20 to 30 degrees, sagittal tilt of 10 to 20 degrees dorsally, and radial shortening of 0 to 2 mm. Articular incongruity greater than 2 to 3 mm may also require osteotomy.
Examination/Imaging
Imaging
 Standard anteroposterior, lateral, and oblique radiographs of both wrists are essential for preoperative planning.
Standard anteroposterior, lateral, and oblique radiographs of both wrists are essential for preoperative planning.
 For most deformities, tracings can be made from the anteroposterior and lateral radiographs and superimposed on each other. The angle and precise location of the deformity can be identified in the frontal and sagittal planes (Fig. 80-4).
For most deformities, tracings can be made from the anteroposterior and lateral radiographs and superimposed on each other. The angle and precise location of the deformity can be identified in the frontal and sagittal planes (Fig. 80-4).
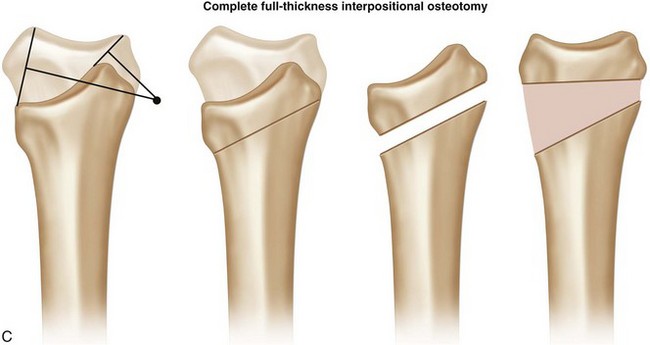
 By superimposing the tracings in the sagittal and frontal planes and drawing a line from the most volar and dorsal lips, a perpendicular line can be drawn midpoint on each line. Where these two intersect will define the type of osteotomy required and the need for lengthening of the distal fragment (Fig. 80-5).
By superimposing the tracings in the sagittal and frontal planes and drawing a line from the most volar and dorsal lips, a perpendicular line can be drawn midpoint on each line. Where these two intersect will define the type of osteotomy required and the need for lengthening of the distal fragment (Fig. 80-5).
Timing
 Osteotomy can be considered when no soft tissue trophic changes or swelling exist, radiographs show limited disuse osteopenia, and digital motion is recovered.
Osteotomy can be considered when no soft tissue trophic changes or swelling exist, radiographs show limited disuse osteopenia, and digital motion is recovered.
 In the absence of trophic changes, early surgical intervention (6 to 12 weeks postinjury) can facilitate correction through incompletely ossified fracture callous, minimize the development of soft tissue contracture and distal radioulnar joint stiffness, and limit the duration of economic and psychological impact on the patient.
In the absence of trophic changes, early surgical intervention (6 to 12 weeks postinjury) can facilitate correction through incompletely ossified fracture callous, minimize the development of soft tissue contracture and distal radioulnar joint stiffness, and limit the duration of economic and psychological impact on the patient.
Exposures
Volar
 The distal part of the anterior Henry approach involves exposure between the flexor carpi radialis and radial artery (Fig. 80-6).
The distal part of the anterior Henry approach involves exposure between the flexor carpi radialis and radial artery (Fig. 80-6).
 The muscle belly of the flexor pollicis longus is retracted ulnarly to expose the pronator quadratus, which is elevated from its insertion on the radius (Fig. 80-7).
The muscle belly of the flexor pollicis longus is retracted ulnarly to expose the pronator quadratus, which is elevated from its insertion on the radius (Fig. 80-7).
 Exposure and realignment of the distal fragment are improved by Z-lengthening of the tendon of the brachioradialis.
Exposure and realignment of the distal fragment are improved by Z-lengthening of the tendon of the brachioradialis.
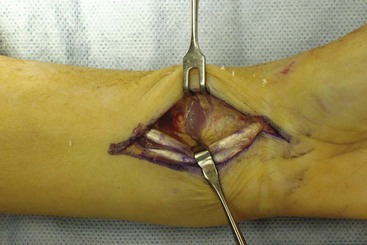
 Small Hohmann retractors are placed along the borders of the distal radius at the site of the deformity (Fig. 80-8).
Small Hohmann retractors are placed along the borders of the distal radius at the site of the deformity (Fig. 80-8).
Dorsal
 The skin incision is between 6 and 8 cm extending 2 to 3 cm distal to the Lister tubercle (Fig. 80-9).
The skin incision is between 6 and 8 cm extending 2 to 3 cm distal to the Lister tubercle (Fig. 80-9).
 Opening the extensor retinaculum can be done either between the second and third or between the third and fourth extensor compartments.
Opening the extensor retinaculum can be done either between the second and third or between the third and fourth extensor compartments.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree