Chapter 8 Implant Pocket Locations
Implant pocket location determines the quality and quantity of long-term soft tissue coverage of breast implants, the number one priority in breast augmentation. Assuring optimal soft tissue coverage of implants for the patient’s lifetime is the number one priority in breast augmentation in order to avoid irreversible tissue compromises and uncorrectable deformities such as visible implant edges and visible traction rippling. No decision in breast augmentation is more important than selection of implant pocket location.
Choice of pocket location and surgical techniques determines the thickness of soft tissue overlying the superior, medial, and inferior areas of every patient’s breast implants for the patient’s lifetime. Inferolaterally and laterally, surgeons have fewer options to increase soft tissue coverage. In areas where additional soft tissue coverage options are available, surgeons should prioritize providing maximal soft tissue coverage above all other considerations or perceived tradeoffs of one pocket location over another.
Subjective Versus Objective Selection of Pocket Location
Objective selection of implant pocket location requires that surgeons do the following:
Implant Pocket Location Options
Retromammary Pocket Location
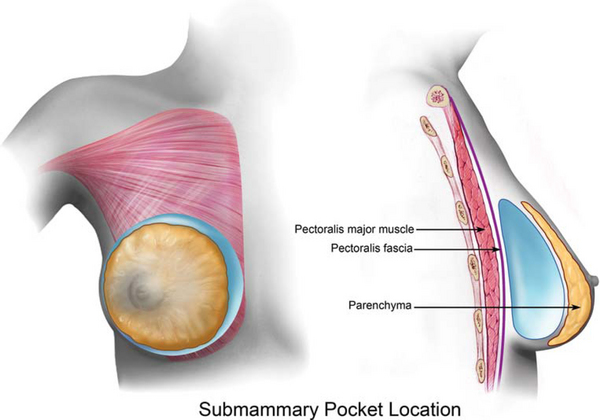
A submammary or retromammary pocket locates the breast implant posterior to the patient’s breast parenchyma and anterior to the pectoralis major muscle and fascia (Figure 8-1). An often quoted advantage of the subpectoral pocket is that it locates the implant in the same tissue plane as the patient’s existing breast parenchyma where the implant is not subject to tissue pressures and tissue dynamics of an overlying muscle tissue layer. Absent additional tissue thickness layers on the implant, the implant can exert more direct and predictable fill and pressure to more predictably control breast shape, especially fill in the upper and medial breast areas. The decades long problem with this argument in favor of the submammary pocket location is that it ignores the most important single priority in breast augmentation—maximizing soft tissue cover over the implant for the patient’s lifetime to avoid uncorrectable tissue compromises and tissue deformities that occur with aging, including tissue thinning, skin stretch, implant edge visibility, and visible traction rippling.
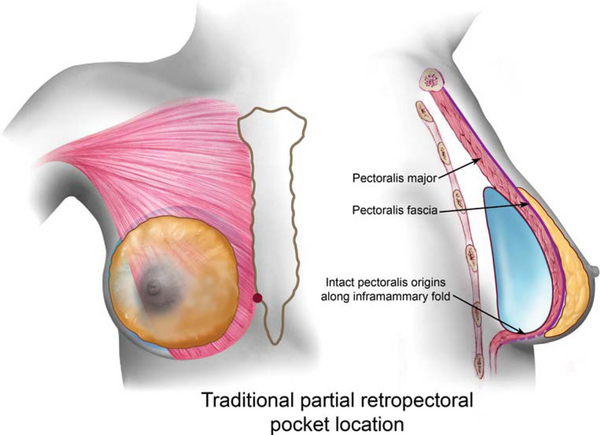
Retromammary placement also theoretically avoids other tradeoffs of muscle pressure on the implant in the subpectoral plane. With traditional partial retropectoral placement, intact pectoralis origins along the inframammary fold allow the pectoralis muscle to transmit more pressure to the implant, and can contribute to upward implant displacement (or failure of the implant to rest at exactly the lower border of the pocket), less control of upper and medial fill, and lateral displacement of the implant over time. Dual plane placement,1 discussed in more detail later in this chapter, releases the origins of the pectoralis along the inframammary fold and almost totally obviates these tradeoffs of traditional partial retropectoral placement when compared to submammary placement while providing maximal additional soft tissue coverage medially and superiorly.
Development of the dual plane pocket1 and surgical techniques that minimize trauma to the pectoralis and bleeding,5 combined with tissue based implant selection,2,3 now allow patients with subpectoral and dual plane augmentations to be out to dinner the evening of surgery and return to full normal activities in 24 hours,4,5 a recovery that is indistinguishable from retromammary augmentations
Surgeons have traditionally advised patients that pocket dissection in a submammary plane, because it does not involve dissection beneath the pectoralis muscle, causes less postoperative pain; however, with the development of the dual plane pocket1 and documented 24 hour recovery4,5 using a dual plane pocket, this potential advantage of submammary augmentation is no longer true. Development of the dual plane pocket1 and surgical techniques that minimize trauma to the pectoralis and bleeding,5 combined with tissue based implant selection,2,3 now allow patients with subpectoral and dual plane augmentations to be out to dinner the evening of surgery and return to full normal activities in 24 hours,4,5 a recovery that is indistinguishable from retromammary augmentations. More importantly, for the first time in history a peer reviewed and published study has shown that surgeons can achieve a zero percent reoperation rate in a consecutive series of primary augmentations in an Food and Drug Administration (FDA) premarket approval (PMA) study,6 emphasizing the importance of combining optimal soft tissue coverage, decision processes, and surgical techniques.
In the submammary plane, surgeons can more effectively control the intermammary distance or cleavage gap by dissecting the pockets medially to a desired location that defines a desired intermammary distance. In order to accomplish the same objective in a submuscular plane, surgeons must divide the origins of the pectoralis major muscle medially. In both cases, this apparent benefit can also be a curse longer term. When the medial or inferomedial edge of the implant is covered only by skin and subcutaneous tissue, the thickness of this coverage largely determines whether a patient will experience visible implant edges in the future, and whether visible traction rippling will occur when the weight of the implant pulls on the capsule attached to thin overlying tissues medially. These deformities can sometimes be corrected by changing a submammary implant to a retropectoral pocket location, but at the expense of dealing with additional risks and variables. If a surgeon disrupts or divides the medial origins of the pectoralis muscle along the sternum at any location from sternal notch to xiphoid, visible implant edges and traction rippling are common deformities that are largely uncorrectable. When surgeons markedly narrow the intermammary distance, synmastia risks increase, and synmastia deformities can be extremely difficult or impossible to optimally correct. Patients should be informed and aware that absent extremely thick tissues in the intermammary gap or cleavage gap between the breasts (a very rare occurrence), it is much safer to live with a slightly wider intermammary distance, keeping the medial edge of the implant under existing parenchyma or the pectoralis muscle, rather than living with uncorrectable deformities in the cleavage area.
When capsular contracture rates were extremely high in the 1970s and 1980s with smooth shell implants placed in a submammary location, surgeons began seeking alternatives that included a submuscular pocket location and textured surface implant devices. Over the next three decades, as surgeons used more submuscular pocket locations, an incredibly beneficial byproduct of the first objective to reduce capsular contracture was a dramatic decrease in the incidence of uncorrectable visible implant edges and traction rippling laterally. Uncorrectable deformities that result when surgeons place implants under inadequate or suboptimal soft tissue coverage have occurred since the beginning of breast augmentation, but the direct link between the surgeon prioritizing soft tissue coverage to prevent these problems during the preoperative decision process did not occur until much more recently.1–4
High profile implants placed in the submammary plane place more direct pressure on the breast parenchyma, and are likely to cause more parenchymal atrophy over time when placed submammary compared to subpectoral. The larger the implant and the tighter the overlying skin, the greater the potential extent of parenchymal atrophy. Even moderate profile implants in the submammary plane can cause parenchymal atrophy if implant size is excessive for the dimensions and stretch characteristics of the overlying envelope. These potentially negative effects of implant pressure on parenchyma are actually beneficial when surgeons attempt to correct constriction deformities of the breast, including constricted lower pole breasts and tubular breasts. More direct pressure of the breast implant on constricted parenchyma and the overlying soft tissue envelope promotes stretching and correction of the constricted lower pole tissues, regardless of the type of tissue release the surgeon performs. The dual plane approach discussed later in this chapter facilitates correction of these types of deformity while adding significant additional pectoralis major muscle coverage for the implant superiorly and medially.
Table 8-1 summarizes the potential benefits and inherent tradeoffs of the submammary pocket location.
Table 8-1 Potential advantages and tradeoffs of the submammary pocket location
| Potential advantages* | Potential tradeoffs |
|---|---|
| More direct implant pressure to shape the breast | Inadequate soft tissue coverage superiorly and medially |
| More precise control of upper and medial breast fill | Higher rate of capsular contracture with resultant higher reoperation rates |
| Less risk of lateral displacement of implants due to pectoralis pressure | Greater interference with mammography |
| Less risk of upward displacement of implants due to pectoralis pressure | Increased risk of synmastia with marked narrowing of the intermammary distance |
| Less risk of breast distortion with pectoralis contraction | |
* All of these potential advantages are also achievable using a dual plane pocket location, and the dual plane location maximizes tissue coverage.
Subfascial Pocket Location
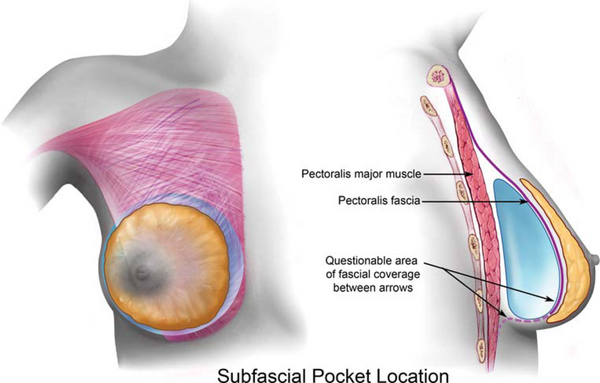
A subfascial pocket locates the breast implant posterior to the patient’s breast parenchyma and posterior to the pectoralis major fascia but anterior to the pectoralis major muscle (Figure 8-2). The subfascial pocket concept was introduced by Graf and associates in 2002.7 In their publication the authors state that potential advantages of a subfascial pocket include: (1) avoiding implant deformation or distortion (as seen in the retromuscular position), (2) leaving additional soft tissue between the implant and the skin, and (3) minimizing implant edge prominence that is, according to the authors, inherent to subglandular placement.
Fresh cadaver anatomy of the pectoralis fascia
The characteristics of the pectoralis fascia are best illustrated in fresh cadaver dissections where the anatomy can be exposed widely under direct vision, facilitating exposure and elevation of the pectoralis fascia unhindered by blood in an operating field which can make the layer almost imperceptible. Embalmed cadaver analysis of the pectoralis fascia is virtually useless as it pertains to clinical reality, because the embalming process totally changes the characteristics of the pectoralis fascia. Analysis of the thickness of the pectoralis fascia, especially in embalmed cadavers, has little pertinence to the key clinical question of whether any surgeon can predictably elevate the pectoralis fascia intact, and even if the surgeon can do that, whether the pectoralis fascia provides scientifically verifiable soft tissue coverage that is really any different compared to a submammary pocket. To date, despite numerous anecdotal reports of clinical series using a subfascial pocket location, no published study has compared scientifically valid cohorts of patients with various pocket locations because no comparative study has controlled for the 53 tissue and surgical variables that exist in every breast augmentation patient.2
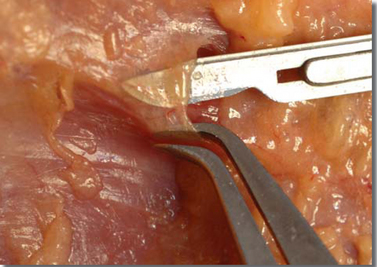
Figure 8-3 is a lateral view of the right breast in a fresh cadaver dissection. The pectoralis fascia 3 cm above the inframammary fold has been incised and draped over the tips of Adson forceps. Figure 8-4 is a closeup view of the pectoralis fascia draped over the Adson forceps with the fascia resting between the tips of calipers set at 1 mm thickness. At this level, 3 cm above the inframammary fold, the pectoralis fascia is not more than 0.2 mm thick, and is difficult to maintain intact for draping between the caliper tips.
In the right breast of this cadaver, the author and an assistant attempted to elevate the breast tissue off the underlying pectoralis fascia under direct vision with wide exposure. Figure 8-5 shows the breast parenchyma reflected laterally, exposing the pectoralis major muscle and overlying pectoralis fascia. Small portions of breast and adipose tissue were left attached to the pectoralis fascia in an attempt to preserve the layer intact, but even with this wide exposure under direct vision, it was exceedingly difficult to maintain the pectoralis fascia intact. Small disruptions of the fascia are apparent in several areas of the dissection.
The pectoralis fascia is supposedly thickest over the middle and upper portions of the pectoralis major muscle. In Figure 8-6, the scalpel has made a small incision in what appears to be the thickest portion of the fascia over the upper portion of the muscle. This area would be the thickest portion of pectoralis fascia overlying a subfascial breast implant. Figure 8-7 is a closeup photograph of the fascia draped over the tip of the scalpel blade. The fascia is so thin that it is transparent, allowing the cutting edge of the scalpel blade to show through the fascia. In Figure 8-8 the fascia on one side of the incision has been placed between caliper tips with the caliper set at 1 mm. The thickness of the pectoralis fascia over this upper portion of the pectoralis muscle is clearly in the range of 0.1–0.2 mm at most, and the filmy, flimsy tissue characteristics of the fascia are apparent.
The photographs of fresh cadaver illustrations in this chapter, combined with basic clinical observation during breast augmentation and reconstruction, should convince any surgeon that the pectoralis fascia is not a tissue layer that provides any meaningful, additional soft tissue coverage over any breast implant compared to a submammary placement. In no area overlying a breast implant does the amount of coverage added by pectoralis fascia compare with pectoralis major muscle coverage. These observations can be confirmed in any clinical case of breast augmentation or reconstruction by simply examining the pectoralis fascia in various areas. The appeal of a subfascial pocket to some surgeons, regardless of the reasons, is anatomically illogical and scientifically unproved.
Advantages and tradeoffs of a subfascial pocket location
The potential positives of the subfascial pocket location are much more theoretical than real. The subfascial pocket is essentially a submammary pocket with at most 1 mm of additional fascial coverage. The pectoralis fascia is thickest superiorly (and less than 1 mm thick in that location), and thins significantly from the mid level of the muscle inferiorly to become almost non-existent near the inframammary fold. In most cases the pectoralis inferiorly is indistinguishable from the deep subcutaneous fascia at the level of the inframammary fold. Surgeons can readily observe the thickness and tissue characteristics while performing breast augmentation or reconstruction procedures, and can easily appreciate the difficulty of raising this particularly thin and flimsy layer of fascia intact. In addition, the pressure and stretch forces exerted by even a moderate size breast implant render this tissue layer even thinner and of no significance whatever as additional soft tissue cover.
Table 8-2 summarizes the potential benefits and inherent tradeoffs of the subfascial pocket location.
Table 8-2 Potential advantages and tradeoffs of the subfascial pocket location
| Potential advantages | Potential tradeoffs |
|---|---|
| Less risk of lateral displacement of implants due to pectoralis pressure | Thin, flimsy tissue layer that provides no additional soft tissue coverage superiorly and medially—less than an additional 1 mm of fascia is not meaningful coverage |
| Less risk of upward displacement of implants due to pectoralis pressure | No proof that fascia can be dissected intact to provide complete implant coverage, especially inferiorly |
| Less risk of breast distortion with pectoralis contraction | Greater interference with mammography |
| 1 mm or less additional coverage compared to submammary | Increased risk of synmastia with marked narrowing of the intermammary distance |
| Decreased risks of implant edge prominence compared to submammary | No published data with preop and postop tissue thicknesses documented to prove any advantage |
In summary, the subfascial pocket location provides no proved advantages in valid scientific studies compared to the submammary pocket location, and the thin, flimsy layer of fascia provides no significant additional soft tissue coverage compared to the submammary pocket location.
Partial Retropectoral Pocket Location
A partial retropectoral pocket (traditional “subpectoral” pocket) locates the breast implant posterior to the patient’s breast parenchyma and posterior to the pectoralis major muscle and fascia, and preserves all pectoralis major muscle origins across the inframammary fold area (Figure 8-9). Dempsey and Latham proposed a partial retropectoral or subpectoral pocket location in 19688 and during the next decade many surgeons noted a significant reduction in capsular contracture rates with smooth shell, silicone gel filled implants in the subpectoral location. When developing a traditional subpectoral or partial retropectoral pocket, the surgeon does not divide the inferior origins of the pectoralis major across the inframammary fold.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree