Procedure 8 Acute Repair of Zone 2 Flexor Tendon Injury
![]() See Video 5: Acute Repair of Zone 2 Flexor Tendon Injury
See Video 5: Acute Repair of Zone 2 Flexor Tendon Injury
Figure 8-7 is adapted from Tang JB. Flexor tendon repair in zone 2C. J Hand Surg [Br]. 1994;19:72-75, with permission from Elsevier. Figure 8-18 is adapted from Strickland JW. Development of flexor tendon surgery: twenty-five years of progress. J Hand Surg [Am]. 2000;25:214-235, with permission from Elsevier.
Indications
 Acute repair of zone 2 flexor tendon injuries is indicated when there is a clean-cut injury with the following findings:
Acute repair of zone 2 flexor tendon injuries is indicated when there is a clean-cut injury with the following findings:
 A tendon defect of up to 1 cm can be repaired by end-to-end suturing. Greater losses (up to 2 to 3 cm) may need an intramuscular tendon lengthening via forearm incisions, and larger tendon gaps will need tendon grafting.
A tendon defect of up to 1 cm can be repaired by end-to-end suturing. Greater losses (up to 2 to 3 cm) may need an intramuscular tendon lengthening via forearm incisions, and larger tendon gaps will need tendon grafting.
Examination/Imaging
Clinical Examination
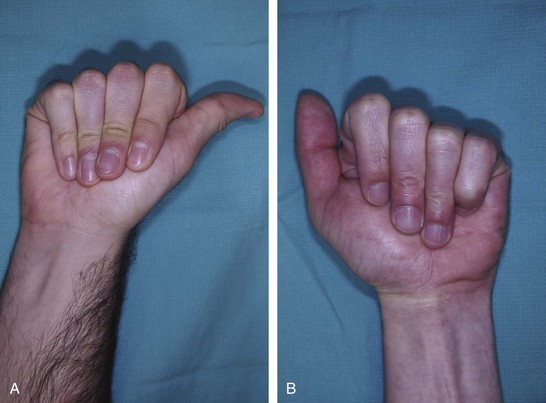
 Patients present with loss of active distal interphalangeal (DIP) and proximal interphalangeal (PIP) joint flexion if both FDP and FDS are divided, or loss of only DIP joint flexion if only FDP has been injured. On inspection, the normal finger cascade is lost with the affected digit in an extended position.
Patients present with loss of active distal interphalangeal (DIP) and proximal interphalangeal (PIP) joint flexion if both FDP and FDS are divided, or loss of only DIP joint flexion if only FDP has been injured. On inspection, the normal finger cascade is lost with the affected digit in an extended position.
 The function of the FDP is determined by asking the patient to actively flex the DIP joint of the involved finger.
The function of the FDP is determined by asking the patient to actively flex the DIP joint of the involved finger.
 Testing for FDS injury is more complex compared with the FDP because the PIP joint is flexed both by the FDS and by the FDP. Therefore, one needs to check the function of the FDS while blocking the action of the FDP.
Testing for FDS injury is more complex compared with the FDP because the PIP joint is flexed both by the FDS and by the FDP. Therefore, one needs to check the function of the FDS while blocking the action of the FDP.
 A partial tendon laceration should be suspected in patients in whom active motion is associated with pain or triggering.
A partial tendon laceration should be suspected in patients in whom active motion is associated with pain or triggering.
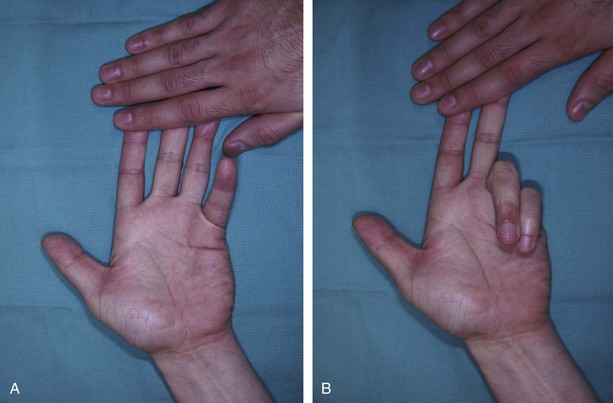
 In patients who cannot cooperate (e.g., children or comatose or intoxicated patients), one can look for passive movement of the fingers resulting from the wrist tenodesis effect or by squeezing the forearm muscles (Fig. 8-5). The same maneuvers can be used when trying to differentiate between tendon injury and inability to move as a result of nerve palsy.
In patients who cannot cooperate (e.g., children or comatose or intoxicated patients), one can look for passive movement of the fingers resulting from the wrist tenodesis effect or by squeezing the forearm muscles (Fig. 8-5). The same maneuvers can be used when trying to differentiate between tendon injury and inability to move as a result of nerve palsy.
 It is important to examine the patient for presence of concomitant injuries to the digital arteries and nerves.
It is important to examine the patient for presence of concomitant injuries to the digital arteries and nerves.
Imaging
 Preoperative imaging studies are not typically necessary, but anteroposterior and lateral x-rays may help identify associated bony injury. When a patient presents with unstable or intra-articular fractures, rigid fixation of the fracture is performed so that judicious tendon mobilization can be performed after tendon repair.
Preoperative imaging studies are not typically necessary, but anteroposterior and lateral x-rays may help identify associated bony injury. When a patient presents with unstable or intra-articular fractures, rigid fixation of the fracture is performed so that judicious tendon mobilization can be performed after tendon repair.
Surgical Anatomy
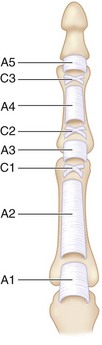
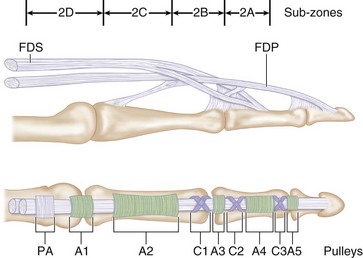
 Zone 2 contains both the FDS and FDP tendons and extends from the proximal edge of the A1 pulley in the palm to the insertion of the FDS over the middle phalanx. It includes four annular pulleys (A1, A2, A3, and A4) and two cruciate pulleys (C1 and C2) (Fig. 8-6).
Zone 2 contains both the FDS and FDP tendons and extends from the proximal edge of the A1 pulley in the palm to the insertion of the FDS over the middle phalanx. It includes four annular pulleys (A1, A2, A3, and A4) and two cruciate pulleys (C1 and C2) (Fig. 8-6).
 Zone 2 was subdivided by Tang (1994) into four subzones (Fig. 8-7).
Zone 2 was subdivided by Tang (1994) into four subzones (Fig. 8-7).
 The blood supply to the tendons in this region comes from the vincular system and enters the tendon on the dorsal surface. It is recommended that core sutures be passed in the palmar portion of the tendon.
The blood supply to the tendons in this region comes from the vincular system and enters the tendon on the dorsal surface. It is recommended that core sutures be passed in the palmar portion of the tendon.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree