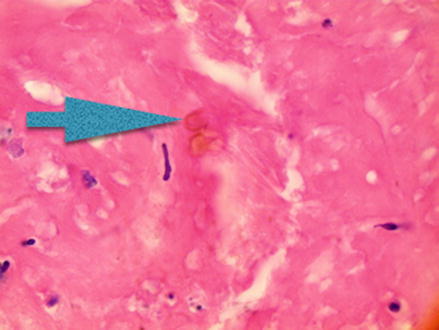
Figure 25.1
Chromoblastomycosis infection of the arm
Clinical Differential Diagnosis
Bacteria abscess
Fungal infection (Chromoblastomycosis)
Diagnosis
CHROMOBLASTOMYCOSIS is a chronic fungal infection that occurs in the cutaneous and subcutaneous tissues of the lower extremities. It characteristically affects middle-aged men with agricultural occupations in tropical and subtropical climates like Madagascar, Australia, China, Mexico, Cuba, and Africa.
Chromoblastomycosis presents as painless red to violaceous, verrucous papules or plaques with satellite lesions that spread in a centripetal fashion. They are often described as cauliflower-like in appearance. Lesions that have been present for a long time may demonstrate an annular pattern with central clearing. They are usually not painful but can be pruritic and bleed easily when traumatized. Typically only one of the lower extremities is involved but there are cases of upper limb and trunk involvement in non-agricultural areas. One Japanese study of 290 chromoblastomycosis lesions reported that the majority of lesions were found on the upper extremities of men and the faces and necks of women.
Several pigmented (dematiaceous) fungi are responsible for this disease; however Fonsecaea pedrosoi is the most common cause and is responsible for more than 80 % of the infections. The other fungi responsible for the remainder of the cases include: Cladosporium carrionii, Fonsecaea compacta, Fonsecaea monophora, Phialophora verrucosa, and Rhinocladiella aquaspersa. They all produce the characteristic sclerotic bodies (referred to as either Medlar, copper penny or muriform bodies) that can be found intracellularly in macrophages or extracellularly in abscesses.
These fungi are found in soil, plants, and decaying vegetation. Chromoblastomycosis is acquired most commonly by traumatic inoculation. The classic history is an agricultural worker who reports a nodule that formed at the site of a splinter puncture. These lesions usually present 1–2 months after inoculation. Chromoblastomycosis is a slow growing, locally progressive disease that can spread by autoinoculation or through the lymphatic system. Complications of this disease include lymphedema, ulceration, and secondary bacterial infection. Rare cases of malignant transformation to squamous cell carcinoma and melanoma have been reported. These cases occurred after more than 10 years of disease duration.
The diagnosis can be made using direct microscopy, culture, or histopathology. A KOH scraping of the black dots visible on the lesion will demonstrate the characteristic brown sclerotic cells with thick walls that are pathognomonic for chromoblastomycosis (Fig. 25.2). Occasionally dark thick hyphae are identifiable, as well. A culture may then be used to determine the specific fungal species. A biopsy will show a granulomatous lesion with sclerotic bodies and an epidermis that is thickened due to a process known as pseudoepitheliomatous hyperplasia. A host response process referred to as transepithelial elimination occurs when dermal fungi material and damaged tissue are expelled through the epidermis. The visible characteristic black dots on the surface of the lesions are the result of this process and represent fungal and necrotic debris.