Procedure 71 Open Reduction and Acute Repair of Perilunate Fracture-Dislocations
Examination/Imaging
Clinical Examination
 Severe wrist edema, tenderness, and ecchymosis may accompany the extreme pain that the patient is experiencing.
Severe wrist edema, tenderness, and ecchymosis may accompany the extreme pain that the patient is experiencing.
 Passive wrist motion is usually limited, painful, and disjointed (not smooth).
Passive wrist motion is usually limited, painful, and disjointed (not smooth).
 It is essential that a thorough neurovascular examination be performed to rule out acute carpal tunnel syndrome.
It is essential that a thorough neurovascular examination be performed to rule out acute carpal tunnel syndrome.
 If numbness, tingling, and two-point discrimination worsen after closed reduction, immediate carpal tunnel release should be performed (along with open reduction and fixation).
If numbness, tingling, and two-point discrimination worsen after closed reduction, immediate carpal tunnel release should be performed (along with open reduction and fixation).
 If the neurovascular examination is improving or normal and a good reduction is achieved, the surgery can be performed electively.
If the neurovascular examination is improving or normal and a good reduction is achieved, the surgery can be performed electively.
Imaging
 Lunate and perilunate dislocations are occasionally missed in the emergency room and dismissed as a severe wrist sprain despite having adequate imaging. Therefore, it is essential to obtain a thorough radiographic examination and scrutinize the images to prevent missing an acute injury.
Lunate and perilunate dislocations are occasionally missed in the emergency room and dismissed as a severe wrist sprain despite having adequate imaging. Therefore, it is essential to obtain a thorough radiographic examination and scrutinize the images to prevent missing an acute injury.
 A standard radiographic series of the wrist must be obtained to evaluate for dislocation. Assess for disruption of Gilula arc lines on the posteroanterior image. On a lateral radiograph, the radial shaft, lunate, capitate, and metacarpal shafts should be collinear (Fig. 71-1).
A standard radiographic series of the wrist must be obtained to evaluate for dislocation. Assess for disruption of Gilula arc lines on the posteroanterior image. On a lateral radiograph, the radial shaft, lunate, capitate, and metacarpal shafts should be collinear (Fig. 71-1).
 Radiographs should also be inspected to rule out associated radial styloid, scaphoid, capitate, or triquetral fractures (Fig. 71-2).
Radiographs should also be inspected to rule out associated radial styloid, scaphoid, capitate, or triquetral fractures (Fig. 71-2).
 Computed tomography can help better define any questionable fractures of the carpal bones.
Computed tomography can help better define any questionable fractures of the carpal bones.
Surgical Anatomy
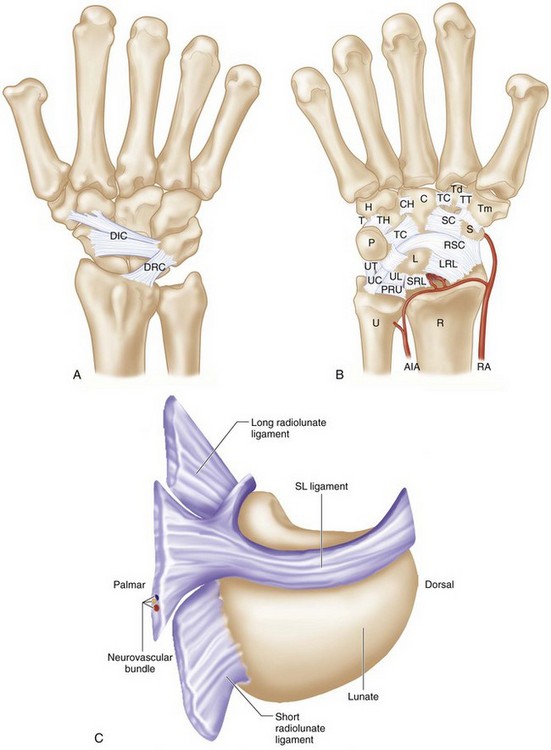
 The dorsal radiocarpal and intercarpal ligaments are frequently ruptured in these severe injuries (Fig 71-3A).
The dorsal radiocarpal and intercarpal ligaments are frequently ruptured in these severe injuries (Fig 71-3A).
 The strong volar ligaments have a characteristic transverse rent that is repaired through the volar approach (Fig. 71-3B).
The strong volar ligaments have a characteristic transverse rent that is repaired through the volar approach (Fig. 71-3B).
 The lunate dislocates through the space of Poirier, a relatively weak region of the volar capsule just below the arc of the radioscaphocapitate and ulnocapitate ligaments (see Fig. 71-3B).
The lunate dislocates through the space of Poirier, a relatively weak region of the volar capsule just below the arc of the radioscaphocapitate and ulnocapitate ligaments (see Fig. 71-3B).
 The dorsal portion of the scapholunate ligament is the thickest and strongest portion of the C-shaped ligament and should be repaired if adequate ligament tissue is present (Fig. 71-3C).
The dorsal portion of the scapholunate ligament is the thickest and strongest portion of the C-shaped ligament and should be repaired if adequate ligament tissue is present (Fig. 71-3C).
 The short radiolunate ligament serves as the pivot for the lunate when it dislocates into the carpal tunnel. It also provides blood supply to the dislocated lunate to prevent avascular necrosis.
The short radiolunate ligament serves as the pivot for the lunate when it dislocates into the carpal tunnel. It also provides blood supply to the dislocated lunate to prevent avascular necrosis.
Positioning
 The patient is positioned supine on the operating room table with the arm abducted on a radiolucent hand table.
The patient is positioned supine on the operating room table with the arm abducted on a radiolucent hand table.
 A minifluoroscope is positioned vertically at the end of the hand table with the image intensifier under the table.
A minifluoroscope is positioned vertically at the end of the hand table with the image intensifier under the table.
 Five to 10 pounds of longitudinal traction using finger traps may be helpful to obtain and maintain lunate reduction and proper position of the carpal bones.
Five to 10 pounds of longitudinal traction using finger traps may be helpful to obtain and maintain lunate reduction and proper position of the carpal bones.