Figure 5.1
Herpes Zoster, note the dermatome distribution

Figure 5.2
Herpes zoster, vesicles themselves appear the same as herpes simplex

Figure 5.3
Herpes Zoster, note the grouped vesicles in this resolved lesion
Clinical Differential Diagnosis
Drug eruption
Herpes Zoster with follicular involvement
Bullous pemphigoid
Stasis blister
Histopathology
A shave biopsy was taken from the right lower leg and it measured 0.7 × 0.5 × 0.1 cm. Sections showed extensive acantholysis and necrosis of the keratinocytes. Nuclear molding and margination were also noted within the follicular epithelium as well.
Diagnosis
HERPES ZOSTER WITH FOLLICULAR INVOLVEMENT. This lesion represents reactivation of varicella (chicken pox). After the initial infection, the virus is integrated within the nerve nucleus, only to re-emerge when cell mediate immunity is weakened. Natural aging, those over 50 years old face a slow decline in the cellular immunity so the risk of herpes zoster rises over time. Pain is the most common complication (post-herpetic neuralgia). Folliculitis is defined as inflammation of the hair follicle. When herpes simplex virus or varicella zoster virus infects the hair follicle, the result is herpes folliculitis (Fig. 5.4). This is a rare diagnosis, there are less than 30 reported cases of herpes folliculitis in the literature. It is difficult for dermatologists to determine that a virus is the cause of the folliculitis based solely on the clinical presentation. Usually the diagnosis is not made until treatments for bacterial and fungal folliculitis have failed. At that point, the work up progresses until the viral cause is exposed.
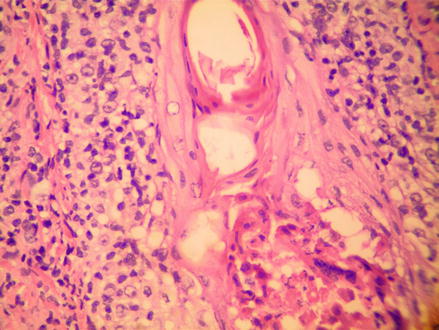
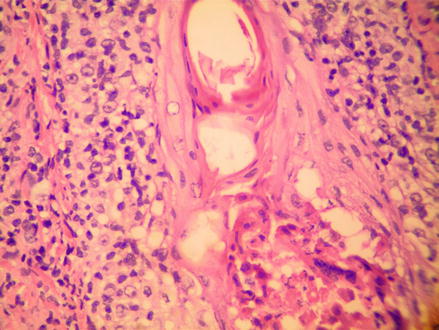
Fig. 5.4
H&E 400×, Herpes folliculitis, HSV changes are found within the follicular epithelium
A typical cutaneous herpetic infection presents as grouped vesicles on an erythematous base. These vesicles evolve into pustules that eventually rupture and form an overlying crust. The lesions can be pruritic and painful. Herpes folliculitis, however, does not present as a typical herpetic infection. Rather it assumes the guise of a characteristic folliculitis with folliculocentric papules or pustules on an erythematous base. In the past, herpes folliculitis was thought to be caused by the herpes simplex virus (HSV-1 or HSV-2). Recent literature argues that herpes folliculitis is more common in patients who have a varicella zoster virus (VZV) infection than a HSV infection. Using polymerase chain reaction studies for specific DNA, a study by Boer et al. demonstrated that out of 21 subjects diagnosed with herpes folliculitis, 17 tested positive for VZV, four were positive for HSV-1, and none tested positive for HSV-2.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








