Procedure 70 Medial Femoral Condyle Vascularized Bone Flap for Scaphoid Nonunion
![]() See Video 52: Free Medial Femoral Condyle Vascularized Bone Transfer for Scaphoid Nonunion
See Video 52: Free Medial Femoral Condyle Vascularized Bone Transfer for Scaphoid Nonunion
Indications
 The main indication is a history of previously failed bone grafting, with plain radiographic and magnetic resonance imaging (MRI) evidence of avascular necrosis associated with scaphoid foreshortening.
The main indication is a history of previously failed bone grafting, with plain radiographic and magnetic resonance imaging (MRI) evidence of avascular necrosis associated with scaphoid foreshortening.
 If there are intraoperative findings showing no bleeding from the proximal and distal scaphoid, it is appropriate to reconstruct the defect with vascularized bone flap.
If there are intraoperative findings showing no bleeding from the proximal and distal scaphoid, it is appropriate to reconstruct the defect with vascularized bone flap.
 Another indication of medial femoral condyle vascularized bone flap is atrophic nonunion of a long bone with a small bone defect that is surrounded by poorly vascularized bed.
Another indication of medial femoral condyle vascularized bone flap is atrophic nonunion of a long bone with a small bone defect that is surrounded by poorly vascularized bed.
 If the nonunion site has punctate bleeding after débridement, corticocancellous wedge bone grafting through the dorsal approach for proximal pole nonunion and through the volar approach for waist nonunion with humpback deformity should be attempted.
If the nonunion site has punctate bleeding after débridement, corticocancellous wedge bone grafting through the dorsal approach for proximal pole nonunion and through the volar approach for waist nonunion with humpback deformity should be attempted.
Examination/Imaging
Imaging
 Posteroanterior (PA), lateral, and oblique radiographs of the hand should be taken to assess any dorsal intercalated segment instability (DISI) deformities or scaphoid foreshortening.
Posteroanterior (PA), lateral, and oblique radiographs of the hand should be taken to assess any dorsal intercalated segment instability (DISI) deformities or scaphoid foreshortening.
 Bone scans are useful in visualizing the fracture 4 hours after injury, but not for detection of a nonunion.
Bone scans are useful in visualizing the fracture 4 hours after injury, but not for detection of a nonunion.
 Computed tomography (CT) scans are useful in assessing pseudoarthrosis and show the extent of bone loss. Furthermore, they can pinpoint the exact position of the fractured fragments and determine whether there is any necrosis of the proximal pole. Humpback deformity may be revealed in sagittal views.
Computed tomography (CT) scans are useful in assessing pseudoarthrosis and show the extent of bone loss. Furthermore, they can pinpoint the exact position of the fractured fragments and determine whether there is any necrosis of the proximal pole. Humpback deformity may be revealed in sagittal views.
 An MRI with intravenous contrast (gadolinium) will help determine proximal pole vascularity. Cartilage erosions and osseous avascular necrosis are evaluated mainly in T1-weighted sequences.
An MRI with intravenous contrast (gadolinium) will help determine proximal pole vascularity. Cartilage erosions and osseous avascular necrosis are evaluated mainly in T1-weighted sequences.
Surgical Anatomy
Recipient Site: Vascular Anatomy of Scaphoid
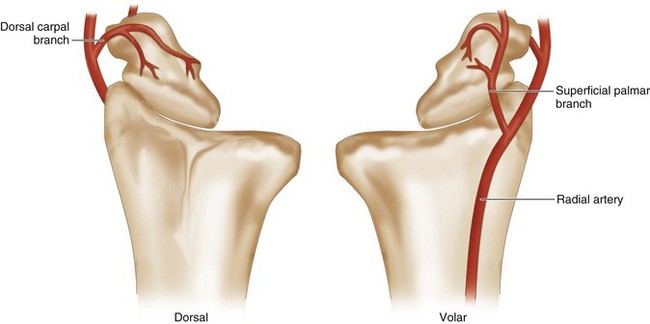
 The major blood supply to the scaphoid is through the radial artery, which enters through the dorsal ridge and supplies 70% to 80% of the intraosseous vascularity to the entire proximal pole. This vessel and its branches enter distally and dorsally in retrograde fashion to the scaphoid. The dorsal vessels travel proximally along the dorsal scaphoid ridge, and the majority of vessels enter the scaphoid waist and continue as intraosseous vessels. The scaphoid proximal pole is uniquely susceptible to avascular necrosis following fracture owing to high dependence on a single dominant retrograde traveling intraosseous vessel (Fig. 70-1).
The major blood supply to the scaphoid is through the radial artery, which enters through the dorsal ridge and supplies 70% to 80% of the intraosseous vascularity to the entire proximal pole. This vessel and its branches enter distally and dorsally in retrograde fashion to the scaphoid. The dorsal vessels travel proximally along the dorsal scaphoid ridge, and the majority of vessels enter the scaphoid waist and continue as intraosseous vessels. The scaphoid proximal pole is uniquely susceptible to avascular necrosis following fracture owing to high dependence on a single dominant retrograde traveling intraosseous vessel (Fig. 70-1).
 Volar radial artery branches provide the blood supply to 20% to 30% of the bone in the region of the distal tuberosity.
Volar radial artery branches provide the blood supply to 20% to 30% of the bone in the region of the distal tuberosity.
Donor Site: Medial Femoral Condyle
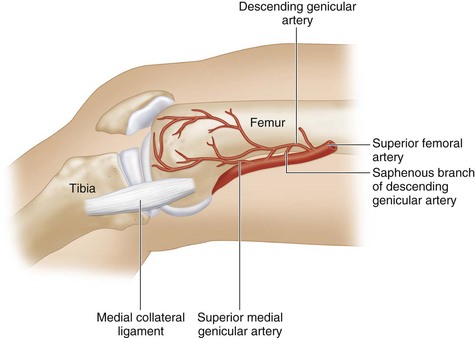
 The superficial femoral artery gives off the descending genicular artery branch just proximal to the adductor hiatus. The descending genicular artery travels distally and gives off a saphenous branch proximally and musculare branches distally. The superior medial genicular artery arises from the superficial femoral artery more distally.
The superficial femoral artery gives off the descending genicular artery branch just proximal to the adductor hiatus. The descending genicular artery travels distally and gives off a saphenous branch proximally and musculare branches distally. The superior medial genicular artery arises from the superficial femoral artery more distally.
 The descending genicular artery and superior medial genicular artery continue distally, penetrate the bone, and provide the blood supply to the medial femoral condyle as intraosseous nutrient vessels.
The descending genicular artery and superior medial genicular artery continue distally, penetrate the bone, and provide the blood supply to the medial femoral condyle as intraosseous nutrient vessels.
 The saphenous branch of the descending genicular artery supplies the medial femoral condyle skin flap (Fig. 70-2).
The saphenous branch of the descending genicular artery supplies the medial femoral condyle skin flap (Fig. 70-2).
Exposures
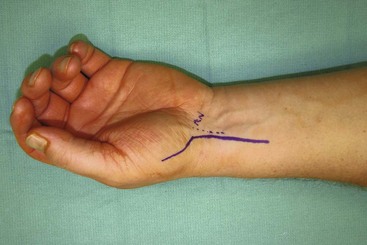
 The scaphoid and radial artery are exposed by a palmar incision. This curvilinear incision extends proximally from the radial aspect of the thenar eminence parallel and radial to the flexor carpi radialis (Fig. 70-3).
The scaphoid and radial artery are exposed by a palmar incision. This curvilinear incision extends proximally from the radial aspect of the thenar eminence parallel and radial to the flexor carpi radialis (Fig. 70-3).
 The medial femoral condyle of the ipsilateral medial knee and its nutrient vessels are exposed using a longitudinal lower medial thigh incision (Fig. 70-4).
The medial femoral condyle of the ipsilateral medial knee and its nutrient vessels are exposed using a longitudinal lower medial thigh incision (Fig. 70-4).
Procedure
Team 1: Donor Site (Bone Graft Harvest)
Step 1
 The femur, patella, and femoral-tibial joint line at the ipsilateral lower medial thigh are marked. A skin incision line centered on the femur from the femoral-tibial joint to the proximal femur is drawn (see Fig. 70-4).
The femur, patella, and femoral-tibial joint line at the ipsilateral lower medial thigh are marked. A skin incision line centered on the femur from the femoral-tibial joint to the proximal femur is drawn (see Fig. 70-4).
Step 2
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree