Procedure 7 Acute Repair of Zone 1 Flexor Digitorum Profundus Avulsion
![]() See Video 4: Acute Repair of Zone 1 Flexor Digitorum Profundus Avulsion
See Video 4: Acute Repair of Zone 1 Flexor Digitorum Profundus Avulsion
Indications
 Loss of flexion of the distal interphalangeal (DIP) joint may occur owing to avulsion of the flexor digitorum profundus (FDP) from its insertion into the distal phalanx.
Loss of flexion of the distal interphalangeal (DIP) joint may occur owing to avulsion of the flexor digitorum profundus (FDP) from its insertion into the distal phalanx.
 Typical etiology is forced extension of the flexed finger, typically when tackling an opponent in football, which is often called “jersey finger.”
Typical etiology is forced extension of the flexed finger, typically when tackling an opponent in football, which is often called “jersey finger.”
 Reattachment is possible if presented 10 to 14 days after injury, or longer if FDP is not retracted proximally because of the restraint provided by the intact vincula.
Reattachment is possible if presented 10 to 14 days after injury, or longer if FDP is not retracted proximally because of the restraint provided by the intact vincula.
 If there is a late presentation, the potential need for tendon grafting or other procedures such as DIP fusion or tenodesis must be discussed.
If there is a late presentation, the potential need for tendon grafting or other procedures such as DIP fusion or tenodesis must be discussed.
 If tendon grafting is contemplated for late presentation, the patient must have a supple DIP joint. In addition, patient expectations must be appropriate.
If tendon grafting is contemplated for late presentation, the patient must have a supple DIP joint. In addition, patient expectations must be appropriate.
Examination/Imaging
Clinical Examination
 With the metacarpophalangeal (MCP) and PIP joints in extension, the patient is unable to actively flex the DIP joint (Fig. 7-1).
With the metacarpophalangeal (MCP) and PIP joints in extension, the patient is unable to actively flex the DIP joint (Fig. 7-1).
 A soft tissue mass may be felt, and there may be localized bruising over the volar finger at the location of the retracted stump.
A soft tissue mass may be felt, and there may be localized bruising over the volar finger at the location of the retracted stump.
Imaging
 Standard anteroposterior and lateral radiographs are necessary.
Standard anteroposterior and lateral radiographs are necessary.
 Lateral radiographs may demonstrate an avulsed bony fragment at the DIP or proximally in the finger or palm corresponding to the proximal retraction of the FDP tendon to which the bone fragment is attached (Fig. 7-2).
Lateral radiographs may demonstrate an avulsed bony fragment at the DIP or proximally in the finger or palm corresponding to the proximal retraction of the FDP tendon to which the bone fragment is attached (Fig. 7-2).
 Ultrasound may be beneficial in confirming the injury, identifying the location of the retracted tendon preoperatively, and aiding in surgical planning, particularly in late presentations.
Ultrasound may be beneficial in confirming the injury, identifying the location of the retracted tendon preoperatively, and aiding in surgical planning, particularly in late presentations.
Surgical Anatomy
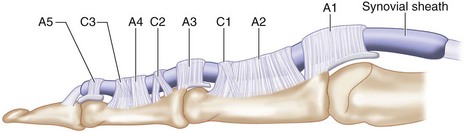
 Flexor zone 1 is distal to flexor digitorum superficialis (FDS) insertion over the middle third of the middle phalanx and contains only the FDP, C3, and A5 pulleys (Fig. 7-3).
Flexor zone 1 is distal to flexor digitorum superficialis (FDS) insertion over the middle third of the middle phalanx and contains only the FDP, C3, and A5 pulleys (Fig. 7-3).
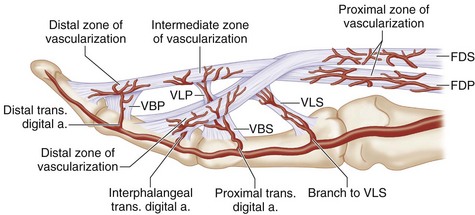
 Blood supply to the distal FDP is from the vinculum longus profundus (VLP), vinculum brevis profundus (VBP), and distal phalanx at its bony insertion (Fig. 7-4).
Blood supply to the distal FDP is from the vinculum longus profundus (VLP), vinculum brevis profundus (VBP), and distal phalanx at its bony insertion (Fig. 7-4).
 Avulsed tendon can retract proximally in three patterns as defined by Leddy and Packer (1977). Additional types 4 and 5 have been described (Fig. 7-5).
Avulsed tendon can retract proximally in three patterns as defined by Leddy and Packer (1977). Additional types 4 and 5 have been described (Fig. 7-5).
 In most cases, the tendon can be retrieved from the above locations, passed through the pulley system, and reattached to the distal phalanx via pullout button or bone anchor.
In most cases, the tendon can be retrieved from the above locations, passed through the pulley system, and reattached to the distal phalanx via pullout button or bone anchor.
 With late presentation of greater than 4 weeks, the myostatic contracture of the avulsed tendon may preclude distal reconstruction, obligating a tendon graft.
With late presentation of greater than 4 weeks, the myostatic contracture of the avulsed tendon may preclude distal reconstruction, obligating a tendon graft.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree