Procedure 64 Diagnostic Wrist Arthroscopy
![]() See Video 48: Diagnostic Wrist Arthroscopy
See Video 48: Diagnostic Wrist Arthroscopy
Indications
 Patients who have objective mechanical pathology of the wrist
Patients who have objective mechanical pathology of the wrist
Examination/Imaging
Clinical Examination
 Arthroscopy has revolutionized the practice of hand surgery by providing the capability to examine and treat intra-articular abnormalities. Development of wrist arthroscopy is a natural transition from the successful application of arthroscopy of the larger joints. Wrist arthroscopy has seen considerable growth since Whipple reported the original description of the technique he developed for reviewing the intra-articular anatomy of the joints.
Arthroscopy has revolutionized the practice of hand surgery by providing the capability to examine and treat intra-articular abnormalities. Development of wrist arthroscopy is a natural transition from the successful application of arthroscopy of the larger joints. Wrist arthroscopy has seen considerable growth since Whipple reported the original description of the technique he developed for reviewing the intra-articular anatomy of the joints.
 A spectrum of injuries is seen in patients with interosseous ligament tears. The interosseous ligament stretches, partially tears, and develops into a full-thickness tear. Patients with scapholunate instability complain of point tenderness directly over the dorsum of the scapholunate ligament. Swelling may be seen localized in this area, and patients may have a positive Watson maneuver. The latter is performed by pushing the tubercle of the scaphoid dorsally with radial wrist deviation. Patients with lunotriquetral interosseous instability complain of point tenderness directly over the dorsum of the lunotriquetral interval. Patients may have a positive shuck test, in which anterior-posterior translation is felt between the lunate and triquetrum, causing point tenderness. A squeeze test consists of radial ulnar compression of the wrist between the thumb and index finger of the examiner. Patients with lunotriquetral instability will complain of pain at the lunotriquetral interval.
A spectrum of injuries is seen in patients with interosseous ligament tears. The interosseous ligament stretches, partially tears, and develops into a full-thickness tear. Patients with scapholunate instability complain of point tenderness directly over the dorsum of the scapholunate ligament. Swelling may be seen localized in this area, and patients may have a positive Watson maneuver. The latter is performed by pushing the tubercle of the scaphoid dorsally with radial wrist deviation. Patients with lunotriquetral interosseous instability complain of point tenderness directly over the dorsum of the lunotriquetral interval. Patients may have a positive shuck test, in which anterior-posterior translation is felt between the lunate and triquetrum, causing point tenderness. A squeeze test consists of radial ulnar compression of the wrist between the thumb and index finger of the examiner. Patients with lunotriquetral instability will complain of pain at the lunotriquetral interval.
 Patients with injury to the TFCC complain of pain at the head of the ulna or the prestyloid recess.
Patients with injury to the TFCC complain of pain at the head of the ulna or the prestyloid recess.
 Patients with fractures of the scaphoid are tender in the snuffbox.
Patients with fractures of the scaphoid are tender in the snuffbox.
 Patients with fractures of the distal radius have generalized swelling around the wrist and are tender to palpation over the distal radius.
Patients with fractures of the distal radius have generalized swelling around the wrist and are tender to palpation over the distal radius.
Imaging
 Multiview radiographs of the wrist on posterior-anterior and lateral planes are mandatory to evaluate for intra-articular pathology.
Multiview radiographs of the wrist on posterior-anterior and lateral planes are mandatory to evaluate for intra-articular pathology.
 Partial tears of the interosseous ligaments are rarely detected on plain radiographs, although dynamic instability may be identified on plain radiographs with dynamic views. Magnetic resonance imaging (MRI) has improved in detecting interosseous injuries. If interosseous ligament injuries are suspected, MRI arthrography is strongly recommended over MRI imaging alone to increase the accuracy of detecting interosseous ligament injuries.
Partial tears of the interosseous ligaments are rarely detected on plain radiographs, although dynamic instability may be identified on plain radiographs with dynamic views. Magnetic resonance imaging (MRI) has improved in detecting interosseous injuries. If interosseous ligament injuries are suspected, MRI arthrography is strongly recommended over MRI imaging alone to increase the accuracy of detecting interosseous ligament injuries.
 Patients with ulnar abutment and central tears of the TFCC can be identified on plain radiographs for patients with a markedly positive ulnar wrist in neutral rotation on radiography.
Patients with ulnar abutment and central tears of the TFCC can be identified on plain radiographs for patients with a markedly positive ulnar wrist in neutral rotation on radiography.
Surgical Anatomy
 The wrist is the labyrinth of eight carpal bones. Multiple articular surfaces with intrinsic and extrinsic ligaments and the TFCC form a perplexing joint that continuously challenges physicians with an array of diagnoses. Wrist arthroscopy allows direct visualization of the cartilage surfaces, carpal bones, and ligaments using bright light and magnification.
The wrist is the labyrinth of eight carpal bones. Multiple articular surfaces with intrinsic and extrinsic ligaments and the TFCC form a perplexing joint that continuously challenges physicians with an array of diagnoses. Wrist arthroscopy allows direct visualization of the cartilage surfaces, carpal bones, and ligaments using bright light and magnification.
 The scapholunate interosseous ligament is best seen with the arthroscope in the 3-4 portal. The lunotriquetral interval is best seen with the arthroscope in the 4-5 or 6R portals owing to its more distal location. The scapholunate interval as seen from the midcarpal space should be tight and congruent. There should be no step-off or separation. The lunotriquetral interval may have slight play between the lunate and the triquetrum. An approximately 1-mm distal step-off of the triquetrum may be seen.
The scapholunate interosseous ligament is best seen with the arthroscope in the 3-4 portal. The lunotriquetral interval is best seen with the arthroscope in the 4-5 or 6R portals owing to its more distal location. The scapholunate interval as seen from the midcarpal space should be tight and congruent. There should be no step-off or separation. The lunotriquetral interval may have slight play between the lunate and the triquetrum. An approximately 1-mm distal step-off of the triquetrum may be seen.
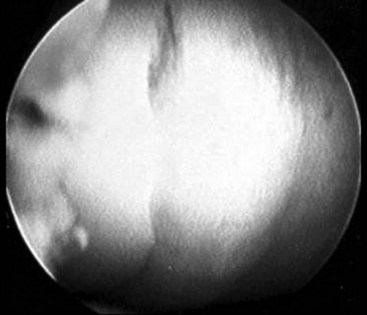
 Geissler defined an arthroscopic classification for interosseous ligament injury. A spectrum of injury is seen throughout this ligament. The ligament stretches and then tears, usually in a volar to dorsal direction. This arthroscopic classification is based on evaluation of the interosseous ligament from both the radiocarpal and midcarpal spaces. (Fig. 64-1 shows arthroscopic view of a normal scapholunate ligament.)
Geissler defined an arthroscopic classification for interosseous ligament injury. A spectrum of injury is seen throughout this ligament. The ligament stretches and then tears, usually in a volar to dorsal direction. This arthroscopic classification is based on evaluation of the interosseous ligament from both the radiocarpal and midcarpal spaces. (Fig. 64-1 shows arthroscopic view of a normal scapholunate ligament.)
Exposures
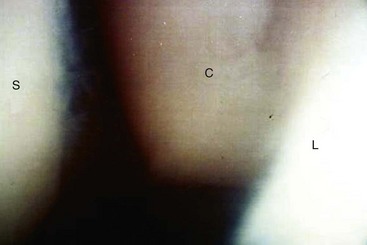
 Wrist arthroscopy portals are made according to the space to which they correspond with respect to the extensor compartments (Fig. 64-6).
Wrist arthroscopy portals are made according to the space to which they correspond with respect to the extensor compartments (Fig. 64-6).
 The traditional portal is the 3-4 portal. This portal is made between the third and fourth dorsal compartments of the wrist. The 3-4 portal is located by palpating Lister tubercle by advancing the finger about 1 cm distal until the soft spot is noted over the dorsal lip of the radius. The 3-4 portal is in line with the radial border of the long finger. (Fig. 64-7
The traditional portal is the 3-4 portal. This portal is made between the third and fourth dorsal compartments of the wrist. The 3-4 portal is located by palpating Lister tubercle by advancing the finger about 1 cm distal until the soft spot is noted over the dorsal lip of the radius. The 3-4 portal is in line with the radial border of the long finger. (Fig. 64-7
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree