Procedure 63 Trapeziometacarpal Fusion
![]() See Video 47: Fusion of Thumb Carpometacarpal Joint
See Video 47: Fusion of Thumb Carpometacarpal Joint
Indications
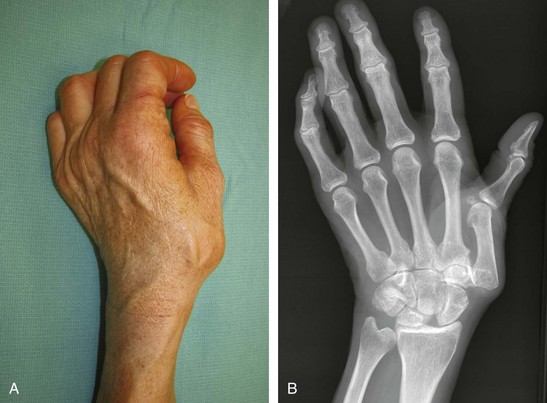
 Posttraumatic degenerative osteoarthritis of the trapeziometacarpal (TMC) joint in manual workers who require great stability of the carpometacarpal (CMC) joint, which may not be achieved with trapezium excision and ligament reconstruction
Posttraumatic degenerative osteoarthritis of the trapeziometacarpal (TMC) joint in manual workers who require great stability of the carpometacarpal (CMC) joint, which may not be achieved with trapezium excision and ligament reconstruction
 Patients with substantial joint laxity and severe thumb CMC joint deformity that cannot be treated with soft tissue reconstruction alone
Patients with substantial joint laxity and severe thumb CMC joint deformity that cannot be treated with soft tissue reconstruction alone
Examination/Imaging
Clinical Examination
 The patient’s thumb should be evaluated for tenderness along the TMC joint.
The patient’s thumb should be evaluated for tenderness along the TMC joint.
 The grind test is performed with axial compression, flexion, extension, and circumduction of the TMC joint, which should elicit crepitus and pain.
The grind test is performed with axial compression, flexion, extension, and circumduction of the TMC joint, which should elicit crepitus and pain.
 The patient’s thumb metacarpophalangeal (MCP) joint should be assessed during pinch for hyperextensibility that can be corrected with MCP joint capsulodesis.
The patient’s thumb metacarpophalangeal (MCP) joint should be assessed during pinch for hyperextensibility that can be corrected with MCP joint capsulodesis.
 The Allen test should be performed because the procedure typically requires mobilization of and potential injury to the radial artery.
The Allen test should be performed because the procedure typically requires mobilization of and potential injury to the radial artery.
Surgical Anatomy
 The TMC joint is a biconcave saddle-shaped joint that provides motion in several planes to allow thumb flexion, extension, abduction, adduction, and opposition.
The TMC joint is a biconcave saddle-shaped joint that provides motion in several planes to allow thumb flexion, extension, abduction, adduction, and opposition.
 The volar oblique (beak) ligament inserts volarly onto the trapezium from its confluence with articular cartilage on the beak of the thumb metacarpal and is considered the primary stabilizer of the TMC joint. It serves as the main restraint against dorsal translation of the metacarpal on the trapezium, and laxity of the beak ligament increases the risk for degenerative changes seen in the CMC joint due to loss of joint stabilization.
The volar oblique (beak) ligament inserts volarly onto the trapezium from its confluence with articular cartilage on the beak of the thumb metacarpal and is considered the primary stabilizer of the TMC joint. It serves as the main restraint against dorsal translation of the metacarpal on the trapezium, and laxity of the beak ligament increases the risk for degenerative changes seen in the CMC joint due to loss of joint stabilization.
 The radial artery traverses the anatomic snuffbox and overlies the dorsal capsule of the CMC joint.
The radial artery traverses the anatomic snuffbox and overlies the dorsal capsule of the CMC joint.
 The abductor pollicis longus (APL) and extensor pollicis brevis (EPB) tendons are within the first extensor compartment.
The abductor pollicis longus (APL) and extensor pollicis brevis (EPB) tendons are within the first extensor compartment.
 The radial sensory nerve becomes subcutaneous after exiting through the interval between the brachioradialis and extensor carpi radialis longus (ECRL) muscles.
The radial sensory nerve becomes subcutaneous after exiting through the interval between the brachioradialis and extensor carpi radialis longus (ECRL) muscles.