Chapter 6 Implants and Implant–Soft Tissue Dynamics
Implant–soft tissue dynamics impact short- and long-term results in breast augmentation. The more a surgeon understands the complex interactions between the implant device and the surrounding and supporting soft tissues, the more predictable the surgeon’s results, and the more optimal the patient’s experience and long-term outcome.
Two categories of breast augmentation exist: breast enlargement (breast stuffing), and breast enlargement (filling and shaping the breast) with optimal control of distribution of fill and long-term aesthetics, while minimizing tissue compromises and reoperations. Stated another way, augmentation can either optimally fill a breast acknowledging breast dimensions and tissue characteristics (“fit and fill”), or the operation can force tissues to a desired result. Optimal long-term aesthetics with minimal tissue compromises and reoperations result when patients and surgeons adopt the “fit and fill” approach, understanding that the dimensions and tissue characteristics of the breast determine optimal implant volume and type. When patients and surgeons do not prioritize tissues above arbitrary wishes, the surgeon may create a desired size and aesthetic appearance, but long-term, the patient may experience compromised aesthetics, additional reoperations, irreversible tissue consequences, and uncorrectable deformities.
Optimal Breast Fill—What is It?
Optimal fill is different in every breast. The wider a breast and the greater the skin stretch, the greater fill is required for an optimal aesthetic result (Figure 6-1). Optimal fill, however, is more than simply the aesthetic result, regardless of whether the aesthetic result appears “natural” or not. The word optimal implies an amount of fill that addresses issues that are equally important compared to any aesthetic considerations. Optimal fill is an amount of fill that recognizes and respects each individual patient’s tissue characteristics, balancing aesthetic considerations with the more important priorities of protecting and preserving the patient’s tissue over her lifetime, and prioritizing optimal soft tissue coverage for the implants long-term. Optimal breast fill is the least amount of fill that will produce the desired aesthetic appearance with the least long-term tissue compromises and the lowest long-term reoperation rates.
Defining Desired Breast Size Preoperatively
Patients frequently attempt to describe their desired breast size by specifying a cup size. Neither surgeons nor patients can define any cup size, and surgeons certainly cannot predictably deliver what they cannot define. Many surgeons also are aware that following augmentation, patients rapidly adjust to their new breast size and then wish they had requested a larger breast. This “if a little is good, more is better” tendency is perhaps a reflection of human nature, but it certainly has been a reality in breast augmentation for decades and has prompted many surgeons to “push” breast size at the primary operation to discourage patients from requesting larger implants postoperatively. This entire line of reasoning by patients and surgeons is severely flawed for several reasons:
Acknowledging these reasoning and decision process flaws, patients nevertheless need to have some understanding of what their result might be before having a breast augmentation. Surgeons are challenged to provide a realistic perspective while attempting to reconcile patients’ wishes with their tissues. While many methods try to achieve these goals, no current methods are optimal based on current reoperation rates for size exchange following breast augmentation. How can surgeons provide a realistic perspective regarding the realities of breast fill and breast size that provides patients an opportunity to elect optimal fill, respecting their tissues, or request and assume full responsibility for a breast size that exceeds the capabilities of their tissues and risks severe tissue compromises?
Most patients, if optimally educated, understand the following concepts:
These questions are absolutely key to the decision making process, because if the patient requests a breast that looks like a normal, natural breast with a full upper pole, then the patient must accept that when the breast envelope is full, it is full, and adding more volume will produce excessive upper bulging that is unnatural and not what she requested. At the same time, if the patient requests a breast that is not empty in the upper pole, the surgeon must place adequate volume in the envelope to fill it, otherwise, the upper breast will be empty.
Helping Patients Understand Breast Size and Fill—the Funnel Analogy
The most effective way to demonstrate these concepts to a patient is to ask the patient to look down while seated in an examination chair. The surgeon grasps the areolar skin and after advising the patient that she may experience some discomfort, pulls the areolar skin maximally anteriorly until the patient experiences discomfort, then marks this point of maximal stretch with the index fingernail of the opposite hand. Releasing the skin, the surgeon then cups the hand around the lower breast at a distance equal to the point of maximal stretch. The dialog with the patient is: “Can you feel that I am pulling your skin as far forward as it is possible to go?” When the patient, wincing, acknowledges positively, the surgeon says: “If I now cup my hand at that maximum stretch distance from your breast, do you understand that your tissues will not stretch much more than what I am showing you?” When the patient acknowledges, the surgeon continues: “As you look down at this approximate amount of enlargement of your breast, do you understand that the amount of expansion of your skin that I am demonstrating is about the maximum stretch your skin can safely tolerate?” The patient, at this point, is acutely aware of the meaning of maximal stretch, based on what she just felt when the surgeon stretched her skin maximally. The surgeon emphatically reminds the patient that although it may be possible to force implant size to further stretch the skin over time, this approach virtually guarantees atrophy or loss of the patient’s breast parenchyma, sacrificing critical coverage over the implant that maximizes risks of visible implant edges and traction rippling, and potentially eliminating the ability of the patient to nurse.
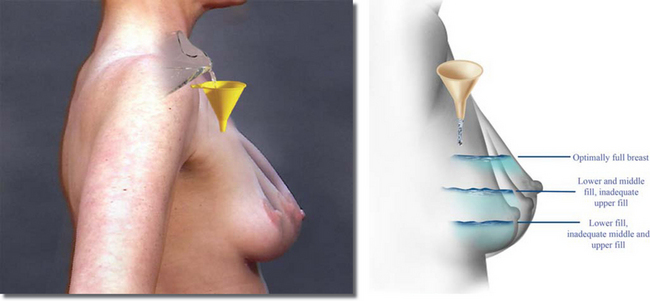
Mentally recording the patient’s reply, the surgeon continues: “If we had a funnel and could simply pour fluid into your breast from above, the lower breast would fill first, then the middle, and finally the top (Figure 6-2). If we stop before we put adequate fill in the breast, the upper breast will not be filled optimally. Once the breast is full and looks perfect, if we continue to add filler, you will have an increasingly bulging and unnaturally appearing upper breast. So, based on the width of your breast and the stretch of your tissue, there is a limit to what we can safely put in your breast and end up with a breast that looks more like a breast compared to a basketball. If you like the rounded, bulging, basketball look, then we must overfill your breast using an excessively large implant, and you must assume full responsibility for tissue changes that might occur over time. These tissue changes can include shrinkage of your breast tissue, thinning of your skin and soft tissue over the implant that allows you to see edges of the implant, tissue thinning that may allow you to see visible traction rippling, and even deformities of your chest wall due to excessive pressure by the implant.”
Controlling Distribution of Fill and Breast Shape
All surgeons address the basic objective of enlarging the breast when they perform breast augmentation. In addition to enlarging the breast, some surgeons also wish to try to improve specific areas of breast shape. Two factors largely determine breast shape: the dimensions and stretch characteristics of the envelope, and the distribution of fill (parenchyma) within the breast envelope. Surgeons cannot change the genetic characteristics of breast skin and the effects of pregnancy on a patient’s breast skin envelope. Surgeons can, however, impact the distribution of fill within the breast and therefore affect breast shape provided they understand three absolute requirements to control breast shape:
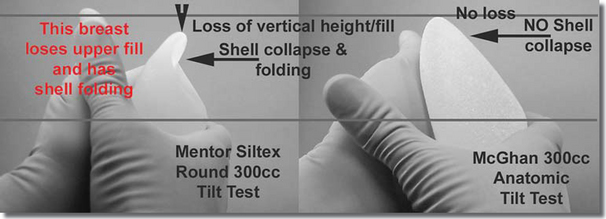
A practical example clarifies these principles. Using any currently manufactured round, smooth, gel or saline breast implant, if the surgeon or manufacturer fills the implant to current manufacturer recommended volumes and the surgeon then performs a tilt test1 on the implant (Figure 6-3, A), the upper pole of the implant collapses because the recommended or actual fill volume of the implant is less than the displacement volume of the mandrel used to manufacture the implant. Manufacturers have traditionally designated round implant recommended fill volumes less than mandrel volume to allow the upper implant to collapse and avoid an excessively round or bulging appearance in the upper breast. While these design and fill parameters may accomplish that goal, surgeons cannot control the distribution of fill within that type of implant. Depending on the degree of “back pressure” on the implant from overlying tissues, the filler within the implant shell can displace in any direction, and in doing so, uncontrollably affect breast shape. With all current round implants, the surgeon cannot control the distribution of the filler within the implant, and because the implant has a smooth outer shell, the surgeon cannot control the position of the implant within the breast pocket. Hence all current round, smooth breast implants fail to satisfy either of the essential criteria that may allow surgeons to control breast shape because surgeons cannot control distribution of fill within the device and they cannot control the position of the device within the breast. In contrast, by increasing the fill to mandrel ratio and refining implant shape, an anatomically shaped, saline filled implant, the Allergan Style 468, does not experience upper shell collapse when tilt tested (Figure 6-3, B). By not experiencing upper shell collapse, the anatomic implant allows the surgeon better control of upper pole fill, and decreases risks of shell folding or collapse that shorten shell life.
To attempt to control breast shape more effectively, surgeons must first control distribution of fill within the implant device. One method of accomplishing this goal is to add more filler to approximate the mandrel volume of the implant. The problem with this method, especially with round implant designs, is that increasing fill produces a shape in the device that is excessively round and causes excessive bulging in the upper breast, compromising surgeons’ ability to produce a natural appearing augmentation result. A second problem, more minor, is an increase in firmness of the device as fill volume increases relative to mandrel volume. Although a concern for some surgeons, peer reviewed and published studies indicate that patients understand and tolerate slight increased firmness if the firmness provides more opportunity to control breast shape and position, and more importantly, to minimize shell collapse and folding that shorten implant shell life.2
The most effective method of controlling distribution of fill within the implant device is to increase the cohesiveness of the filler material. Various materials have been added to saline to attempt to increase its cohesiveness, and all have failed or have caused undesirable side effects that resulted in withdrawal of the products from the market. In contrast, manufacturers can formulate silicone gel to produce a wide range of cohesiveness. A key question is whether increasing cohesiveness of silicone gel filler materials increases control over the distribution of fill within the implant device. The answer is no, unless the degree of cohesiveness increases to a point where the implant becomes form stable when it is subjected to the tilt test. A form stable implant is an implant that experiences no shell folding and minimal, if any, shell collapse, and less than 0.5 cm vertical dimension shortening when a surgeon places the implant in the hand, supports the lower pole without pressing on it, and tilts the implant to an upright position (the tilt test, Figure 6-3, B, right).
The word “cohesive” has become an implant manufacturer marketing buzzword that means little, if anything at all, to the two objectives most important to surgeons and patients: (1) prolonging the life of the implant shell by reducing shell collapse and folding (thereby reducing unnecessary reoperations to replace failed implants), and (2) providing surgeons a device that allows control of distribution of fill within the device that in turn offers more opportunity to control distribution of fill and shape of the breast. One manufacturer, in advertisements, claims that all of their silicone gel implant designs are “all cohesive, all the time”. What the manufacturer does not specify is the actual differences in cohesiveness between their various silicone gel implant products, and how those differences may affect the life of the devices, reoperation rates, and the efficacy of the devices with respect to providing surgeons a better opportunity to control shape in the breast. Even the term “form stable” is becoming polluted by marketing jargon, but implants that meet the criteria for form stability defined previously at least demonstrate control of distribution of fill within the implant shell, and therefore provide surgeons a better opportunity to more accurately control breast shape.
Implant shell characteristics can dramatically affect surgeons’ ability to control the position of the implant in the periprosthetic pocket, and therefore control the distribution of fill in the breast that defines breast shape. Smooth shell implants, regardless of the characteristics of the implant filler material, fall to the most dependent portion of the implant pocket, and provide surgeons virtually no control over distribution of fill within the breast (Figure 6-4), especially the upper breast. Surgeons can increase breast fill by selecting a larger size, smooth shell implant, but surgeons cannot control the distribution of fill within the pocket or within the breast using smooth shell implants.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree