Aggressive Cutaneous Cytotoxic Lymphomas
At the beginning of this chapter, it must be clearly stated that a cytotoxic phenotype does not have any prognostic implication per se, as it can be observed in benign (e.g., pityriasis lichenoides et varioliformis acuta, vitiligo), low-grade malignant (e.g., mycosis fungoides, subcutaneous panniculitis-like T-cell lymphoma), or aggressive cutaneous lymphoproliferative disorders. Thus, demonstration of cytotoxic markers alone does not have any value for the purpose of classification of any given lesion, and only a synthesis of all clinicopathologic features allows a precise diagnosis. It must also be underlined that a cytotoxic profile can be observed in aggressive lymphomas that are not discussed in this chapter (e.g., many cases of cutaneous peripheral T-cell lymphoma, NOS). However, in contrast to peripheral T-cell lymphoma, NOS, which besides a cytotoxic phenotype may also present with a helper or a null-cell phenotype, the three entities included in this chapter always display a cytotoxic phenotype. In addition, they are characterized by overlapping clinicopathologic features that may cause differential diagnostic and classification problems and that are best discussed in a single chapter. Hydroa vacciniforme-like lymphoma is included in Chapter 10 (other cutaneous NK/T-cell lymphomas), because the behaviour is intermediate and the distinctive clinicopathologic features do not pose problems in differential diagnosis with the three lymphoma entities discussed in this chapter.
Primary cutaneous CD8+ epidermotropic aggressive cytotoxic T-cell lymphoma, cutaneous γ/δ T-cell lymphoma, and extranodal NK/T-cell lymphoma, nasal type, show many overlapping clinicopathologic features and classification may be subjective in some cases. In addition, distinction from mycosis fungoides and from subcutaneous panniculitis-like T-cell lymphoma can be difficult or even impossible without proper history and complete clinical information (see also Chapters 2 and 5). In spite of extensive phenotypic and genotypic studies, a few cases may defy precise classification. The main overlapping scenarios among these three lymphoma entities and other NK/T-cell lymphomas can be summarized as follows:
- Cases characterized by the presence of a CD8+ phenotype, epidermotropism of neoplastic cells, and immunohistochemical positivity for TCR-γ (may be included in the group of primary cutaneous aggressive epidermotropic CD8+ cytotoxic T-cell lymphoma or in that of cutaneous γ/δ T-cell lymphoma).
- Cases characterized by immunohistochemical positivity for TCR-γ and by positive in situ hybridization for Epstein–Barr virus (EBV) (EBER-1) (may be included in the group of cutaneous γ/δ T-cell lymphoma or in that of extranodal NK/T-cell lymphoma, nasal type).
- Cases characterized by a T-cell profile consistent with the α/β T-cell variant of extranodal NK/T-cell lymphoma, nasal type, showing a negative reaction for EBER-1 (may be included in the group of extranodal NK/T-cell lymphoma, nasal type, or in that of peripheral T-cell lymphoma, NOS).
- Cases characterized by a phenotypic profile and association with EBV consistent with extranodal NK/T-cell lymphoma, nasal type, occurring in children (may be included in the group of extranodal NK/T-cell lymphoma, nasal-type, or in that of systemic EBV+ T-cell lymphoproliferative disease of childhood).
Although the constellations of findings mentioned above are rare, classification of cases with such features may be subjective. Complete phenotypic investigations usually provide diagnostic clues, but rare cases may defy a precise categorization.
Cytotoxic lymphomas are tumors derived from T or NK lymphocytes with a cytotoxic phenotype. Neoplastic cells typically express at least one cytotoxic protein such as T-cell intracellular antigen (TIA)-1, granzyme B, or perforin. In the World Health Organization (WHO) Classification of Tumours of Haematopoietic and Lymphoid Tissues, extranodal NK/T-cell lymphoma, nasal type, and cutaneous γ/δ T-cell lymphoma are recognized as distinct lymphoma types, whereas primary cutaneous aggressive epidermotropic CD8+ cytotoxic T-cell lymphoma is considered as a provisional entity [1, 2].
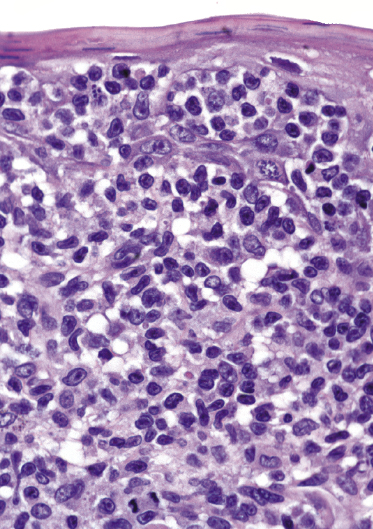
It is important to underline that in aggressive cytotoxic lymphomas cytomorphologic features are variable and are not associated with the clinical outcome. In addition, cytomorphology is similar in all of these entities and may be characterized by predominance of small-, medium-, or large-sized cells (usually with pleomorphic nuclei). Thus, cytomorphologic aspects are neither useful for a specific diagnosis and classification of the lymphoma nor are a feature associated with the biologic behavior, and should always be evaluated together with all other clinical, histopathologic, phenotypic, and molecular genetic features.
Finally, it should be emphasized that distinguishing between primary and secondary cutaneous involvement is less important for these entities than it is for most other skin lymphomas [3–5]. In fact, primary cutaneous cases often develop extracutaneous dissemination within a short period of time, and prognosis is usually very poor regardless of the results of staging investigations at presentation. Thus, although staging investigations are mandatory in all of these patients, treatment should be aggressive even in cases with disease limited to the skin.
Primary Cutaneous Aggressive Epidermotropic CD8+ Cytotoxic T-Cell Lymphoma
Primary cutaneous aggressive epidermotropic CD8+ cytotoxic T-cell lymphoma is a disease characterized by aggressive behavior clinically and proliferation of epidermotropic CD8+ T lymphocytes histopathologically [1, 6, 6a]. Distinction from cases of CD8+ mycosis fungoides and especially from lymphomatoid papulosis type D is made mainly on the basis of the clinical presentation and behavior. In contrast to mycosis fungoides, patients with primary cutaneous aggressive epidermotropic CD8+ cytotoxic T-cell lymphoma present with plaques and tumors, often ulcerated, at the onset of their disease [1, 6–8]. Lymphomatoid papulosis type D is characterized by the typical “waxing and waning” of papules and small nodules (see Chapter 4). A set of diagnostic criteria for primary cutaneous aggressive epidermotropic CD8+ cytotoxic T-cell lymphoma has been proposed, summarizing clinical, histopathologic, and phenotypic features [8].
In the past, cases of primary cutaneous aggressive epidermotropic CD8+ cytotoxic T-cell lymphoma were classified as either aggressive mycosis fungoides (mycosis fungoides “a tumeur d’emblée”) or as generalized pagetoid reticulosis (Ketron–Goodman type). Pediatric patients with a clinical presentation resembling hydroa vacciniforme should be better classified as hydroa vacciniforme-like lymphoma (see Chapter 10).
Clinical Features
The disease occurs in adults of both sexes with a slight male predominance [3, 6]. Only one report on children exists [9]. Patients present with generalized patches, plaques, and tumors, almost invariably ulcerated (Figs 6.1 and 6.2). The clinical features are indistinguishable from those observed in patients with cutaneous γ/δ T-cell lymphoma and are identical to those of generalized pagetoid reticulosis (and of advanced mycosis fungoides) (Fig. 6.3). Involvement of the mucosal regions is common [6]. The tumor often spreads to the central nervous system [6].



As already mentioned, for a diagnosis of primary cutaneous aggressive epidermotropic CD8+ cytotoxic T-cell lymphoma it is crucial to exclude a history of mycosis fungoides or of lymphomatoid papulosis.
Histopathology, Immunophenotype, and Molecular Genetics
Histopathology
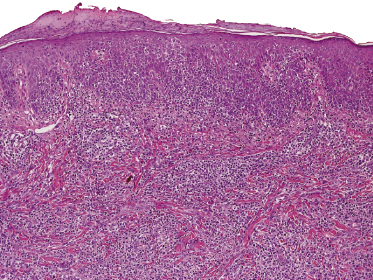
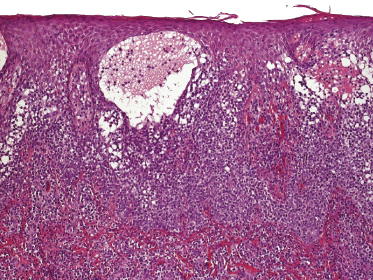
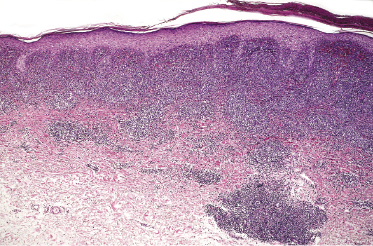
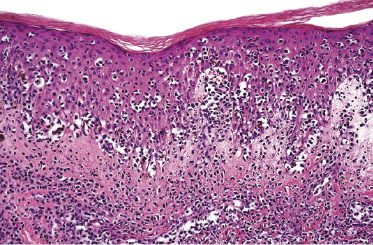
Histology reveals a nodular or diffuse proliferation of lymphocytes with marked epidermotropism (Fig. 6.4). Spongiosis and intraepidermal vesiculation may be observed (Fig. 6.5). In spite of the name of this lymphoma, the epidermotropism may be less pronounced or even missing in some lesions, especially in advanced stages (Fig. 6.6). In such cases, in order to confirm the diagnosis it is necessary to have a previous or concomitant biopsy with typical features of cutaneous aggressive epidermotropic CD8+ cytotoxic T-cell lymphoma. As in all aggressive cutaneous lymphomas, invasion and destruction of adnexal skin structures are common, but angiocentricity and angiodestruction are infrequent. Cytomorphology is variable and can be characterized by small-, medium-, or large-sized pleomorphic cells (Fig. 6.7). Some cases may show a predominance of immunoblasts.
Cases of CD8+ T-cell lymphoma with exclusive involvement of the subcutis should be classified as subcutaneous panniculitis-like T-cell lymphoma. Distinction of primary cutaneous aggressive epidermotropic CD8+ cytotoxic T-cell lymphoma from cutaneous γ/δ T-cell lymphoma is difficult and sometimes determined on an arbitrary basis. Cutaneous γ/δ T-cell lymphoma usually shows a more prominent involvement of the subcutaneous fat. Another differential diagnostic feature is represented by the presence of a marked interface dermatitis in many cases of cutaneous γ/δ T-cell lymphoma. With the exception of the expression of α/β in contrast to γ/δ T-cell receptors, other phenotypic features may be overlapping.
Immunophenotype
Immunohistology reveals a characteristic phenotypic profile of neoplastic lymphocytes (βF1+, CD2−/+, CD3+, CD4−, CD7+, CD8+, TIA-1+, CD45Ra+, CD45RO−) (Figs 6.8 and 6.9) [6]. Some pan-T-cell markers may be lost. In the original description by Berti et al., CD56 was consistently negative [6], but CD56+ cases classified as cutaneous aggressive epidermotropic CD8+ cytotoxic T-cell lymphoma have been described by Santucci et al. [10]. However, in this study cutaneous γ/δ T-cell lymphoma was not included as a specific category, and it may be that these cases represented CD8+ examples of this type of lymphoma.
The EBV is not detectable in neoplastic cells.
Molecular Genetics
Molecular biology shows a monoclonal rearrangement of the T-cell receptor (TCR) genes. No specific genetic alterations have been repeatedly identified. Array comparative genomic hybridization (aCGH) investigations reveal that gains (particularly in chromosomes 3, 7, 8, 11, 17, 18, and 22) are more frequent than losses (these last being found particularly in chromosome 9 at 9p21, suggesting a role of p16).
Treatment
As the disease is very rare, data on therapy are lacking, and double-blinded studies have not been carried out. At present the treatment of choice is systemic chemotherapy. The role of stem cell transplantation has not been evaluated in detail.
Prognosis
The prognosis of patients with primary cutaneous aggressive epidermotropic CD8+ cytotoxic T-cell lymphoma is poor and the estimated 5-year survival is 0% [3, 6]. The median survival is 12 months [6a]. The disease often metastasizes to unusual sites such as the lung, testis, and central nervous system.
Primary Cutaneous γ/δ T-Cell Lymphoma
Primary cutaneous γ/δ T-cell lymphoma is a tumor of cytotoxic γ/δ T lymphocytes with specific tropism for the skin. This lymphoma shows many overlapping features with other cutaneous lymphoma entities, especially with subcutaneous panniculitis-like T-cell lymphoma and with primary cutaneous aggressive epidermotropic CD8+ cytotoxic T-cell lymphoma. Cutaneous γ/δ T-cell lymphoma is included as a distinct entity in the WHO classification [1] and should be distinguished from other γ/δ T-cell lymphomas [11].
The recent availability of a marker for γ/δ T-lymphocytes on routinely fixed, paraffin-embedded sections of tissue (TCR-γ) facilitates the diagnosis of this cytotoxic lymphoma. Although results are not always reliable, in most cases staining for both α/β and γ/δ chains allows a proper classification. In fact, in T-cell lymphomas lack of α/β expression per se is not synonymous with γ/δ differentiation, as “TCR silent” (“null-cell”) cases negative for both α/β and γ/δ may be observed [12]. Besides cutaneous and hepatosplenic cases, γ/δ T-cell lymphomas can be observed rarely also at other nodal or extranodal sites [12], thus underlying the need for staging investigations. It is also important to remember that a γ/δ phenotype is not unique to γ/δ T-cell lymphomas, as it can be observed in several cutaneous (and extracutaneous) lymphoma types, including mycosis fungoides [13].
In the past, cases of cutaneous γ/δ T-cell lymphoma were classified as either generalized pagetoid reticulosis (Ketron–Goodman type) or mycosis fungoides “a tumeur d’emblée.” Distinction from rare cases of conventional mycosis fungoides with γ/δ T-cell phenotype is made exclusively on the basis of the clinical presentation and behavior. In contrast to mycosis fungoides, patients with cutaneous γ/δ T-cell lymphoma present at the onset with rapidly growing, disseminated patches, plaques, and tumors that are often ulcerated.
Due to the frequent prominent involvement of subcutaneous tissues, in the past many cases of cutaneous γ/δ T-cell lymphoma were incorrectly classified as subcutaneous panniculitis-like T-cell lymphoma (see also Chapter 5). However, γ/δ T-cell lymphoma almost invariably shows also prominent involvement of the epidermis either in the same biopsy specimen or in other biopsies taken at the same time or during the course of the disease. A typical example is represented by the patient pictured in Figure 6.10, who was included in the chapter on subcutaneous T-cell lymphomas in the first edition of this book published in 1998 (old Figures 7.1 and 7.2). The same patient was presented as an example of “malignant histiocytosis” in the book on cutaneous lymphomas published in 1983 by Burg and Braun-Falco, who had received the case from Helmut Kerl [14]. The previous classifications made perfect sense at the time when they had been proposed. On the other hand, this case clearly shows how these unusual lymphomas are reclassified over time, thanks to new phenotypic and molecular studies that allow definition of more specific categories. As a matter of fact, staining with the antibody specific for TCR-γ allowed the diagnosis of cutaneous γ/δ T-cell lymphoma to be confirmed more than 36 years after the patient had succumbed to his disease.

Clinical Features
Cutaneous γ/δ T-cell lymphoma occurs in adults, with an equal distribution of males and females. Rare cases in children are well documented [15]. Patients present with localized or generalized patches, plaques, and tumors, which are frequently ulcerated (Fig. 6.11). Localized lesions are often found on the lower extremities. Large, solitary tumors may also be seen. The clinical features are similar to those observed in patients with primary cutaneous aggressive epidermotropic CD8+ cytotoxic T-cell lymphoma and are indistinguishable from those of advanced stages of mycosis fungoides (Fig. 6.12). Some of the patches of the disease, unlike the common patches of mycosis fungoides, may reveal clinical features similar to those of severe interface dermatitis, characterized by a red-brown aspect with small superficial erosions (Fig. 6.13). Involvement of the mucosal regions and of other locations unusual for mycosis fungoides is common (Figs 6.14 and 6.15).





Staging investigations are mandatory and usually show the presence of tumor masses within the soft tissues and/or the lymph nodes. Lactate dehydrogenase (LDH) is elevated in the majority of patients [16]. Bone marrow involvement is uncommon. A hemophagocytic syndrome is a frequent complication.
Almost one-fourth of the patients had an associated autoimmune disorder in one study [16], and onset of cutaneous γ/δ T-cell lymphoma has been observed also during treatment with etanercept for rheumatoid arthritis [17]. In such cases it is difficult to ascertain whether the lymphoma arises in the setting of the autoimmune disorder or as a consequence of the immunomodulatory treatment.
As well as for other aggressive cytotoxic lymphomas, for a diagnosis of cutaneous γ/δ T-cell lymphoma, it is crucial to exclude a history of mycosis fungoides.
Histopathology, Immunophenotype, and Molecular Genetics
Histopathology
Histology reveals a diffuse proliferation of lymphocytes, usually with prominent involvement of the subcutaneous tissues (Fig. 6.16). Epidermotropism is variable and may be marked (Fig. 6.17). In cases with prominent involvement of the subcutaneous tissue, however, the epidermis shows more often features of interface dermatitis with vacuolization of basal keratinocytes and scattered intraepithelial lymphocytes (Fig. 6.18). Although epidermotropic lesions may resemble those observed in mycosis fungoides, unlike mycosis fungoides prominent edema within the papillary dermis is not uncommon in cutaneous γ/δ T-cell lymphoma (Fig. 6.19). Involvement of the dermis also allows a clear morphologic distinction to be made from subcutaneous panniculitis-like T-cell lymphoma, where the dermis is spared as a rule.
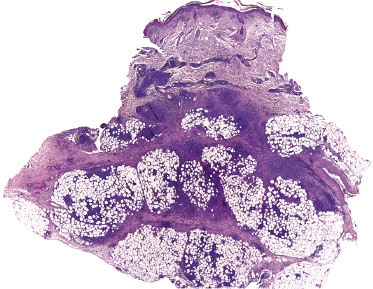
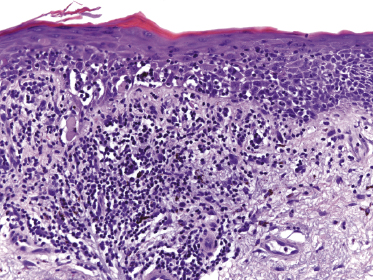
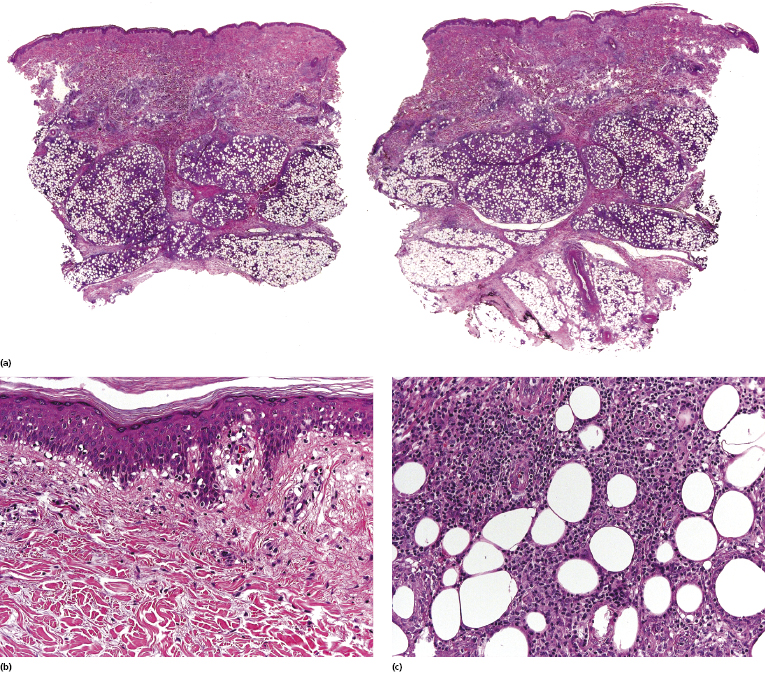
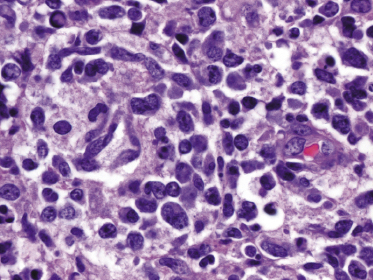
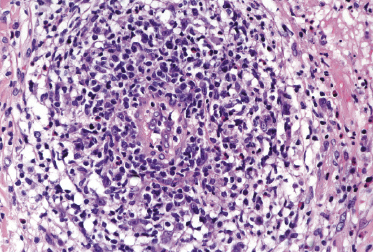
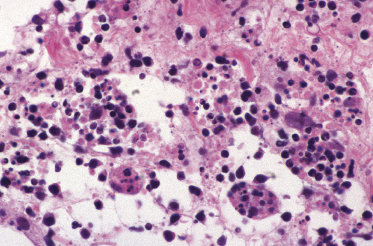
Cytomorphology is variable and can be characterized by small-, medium-, or large-sized pleomorphic cells (Fig. 6.20). Intraepidermal vesiculation and necrosis can be seen. Angiocentricity and/or angiodestruction are a common finding (Fig. 6.21). The presence of large macrophages engulfing neoplastic lymphocytes or other blood cells is a typical feature of cases associated with a hemophagocytic syndrome (Fig. 6.22).
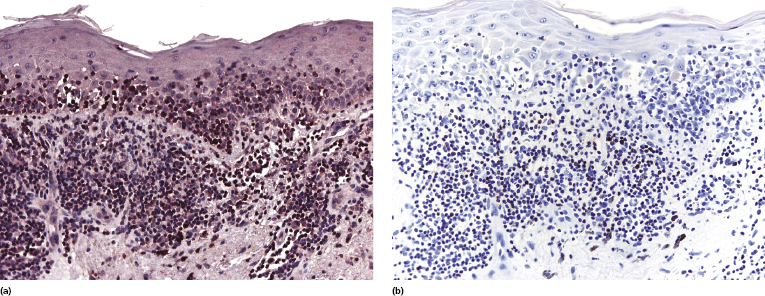
As discussed previously in this chapter, the distinction of cutaneous γ/δ T-cell lymphoma from primary cutaneous aggressive epidermotropic CD8+ cytotoxic T-cell lymphoma may be difficult. Lesions of cutaneous γ/δ T-cell lymphoma show a more prominent involvement of the subcutaneous fat than those of primary cutaneous aggressive epidermotropic CD8+ cytotoxic T-cell lymphoma. Another differential feature is the presence of a marked interface dermatitis in many cases of cutaneous γ/δ T-cell lymphoma, but not in those of primary cutaneous aggressive epidermotropic CD8+ cytotoxic T-cell lymphoma. In cases with marked epidermotropism and positivity for CD8, stainings for α/β and γ/δ allow the two conditions to be distinguished.
Immunophenotype
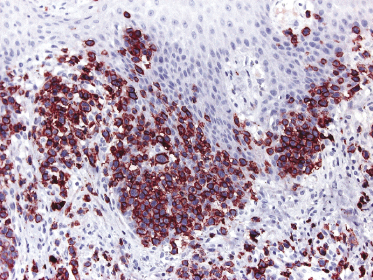
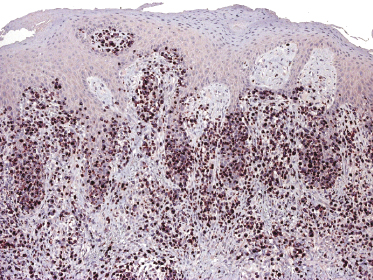
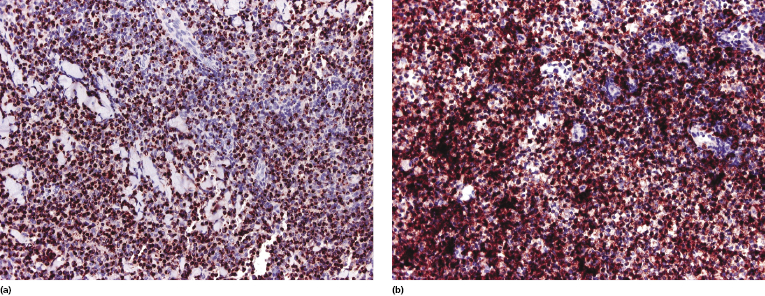
Immunohistology reveals a characteristic phenotypic profile of neoplastic lymphocytes (TCR-γ+, βF1−, CD3+, TIA-1+, CD56+, CD57−) (Fig. 6.23). Stainings for α/β and γ/δ are crucial in order to establish the diagnosis, and often are better evaluated when compared with one another (Fig. 6.24). CD4 is negative, and CD8 may be expressed in some cases. Some pan-T-cell markers may be lost. The proliferation rate (Ki-67) is high, usually >50% and sometimes nearly 100%.
EBV is not present in the neoplastic cells. The classification of rare cases of cutaneous T-cell lymphoma with a γ/δ phenotype and positivity for EBV is a matter of discussion [16, 18, 19]. As already mentioned, the group of cutaneous aggressive cytotoxic lymphomas presents several overlapping features and sometimes classification of a given case may be subjective.
Molecular Genetics
Molecular biology shows a monoclonal rearrangement of the TCR genes. The γ/δ T-cell lymphomas (including both cutaneous and extracutaneous forms) have a different molecular profile than α/β T-cell lymphomas and reveal overexpression of genes of NK-cell-associated molecules such as killer cell immunoglobulin-like receptor (KIR) genes (KIR3DL1, KIR2DL4, and KIR2DL2) and killer cell lectin-like receptor genes (KLRC4, KLRD1, and KLRC2) [20]. In the same study it was shown that hepatosplenic γ/δ T-cell lymphoma represents a tumor distinct from other γ/δ T-cell lymphomas arising at other sites including the skin [20], thus confirming the need for separating different entities of γ/δ T-cell lymphoma.
Chromosomal aberrations suggesting the involvement of a WWOX–TCL gene cluster and BCL11B have been observed in one study [21].
Treatment
Data on therapy are lacking and double-blinded studies have not been carried out. The treatment of choice is systemic chemotherapy. The role of stem cell transplantation has not been evaluated.
Prognosis
The prognosis of patients with cutaneous γ/δ T-cell lymphoma is poor. Occasional patients may show a prolonged course [22, 23]. Involvement of the subcutaneous fat tissues has been related to a bad prognosis [24]. However, as already mentioned, in the group of aggressive cutaneous cytotoxic NK/T-cell lymphomas prognostic features of cases reported in the past may be related to an incorrect classification rather than to genuine features of the neoplasms described. In this context, it has been suggested that expression of the γ/δ phenotype is a bad prognostic indicator in cutaneous T-cell lymphomas irrespective of the classification [24]. However, in our experience a cytotoxic phenotype does not have any prognostic implication in mycosis fungoides (see also Chapter 2) [25].

Full access? Get Clinical Tree


