Figure 16.1
Posterior neck showing folliculitis (Sycosis nuchae)
Clinical Differential Diagnosis
Folliculitis
Adnexal tumor
Cysts
Acne keloidalis
Diagnosis
FOLLICULITIS is defined as inflammation of the pilosebaceous unit (Fig. 16.2). Clinically, it appears as folliculocentric papules or pustules on an erythematous base. Folliculitis can be asymptomatic but the patient may complain of tenderness, pain or pruritus. If the pruritus becomes generalized it is referred to as “itching folliculitis.” Typically the lesions are distributed in areas where terminal hairs are found such as the scalp, beard, upper trunk, buttocks and lower extremities.
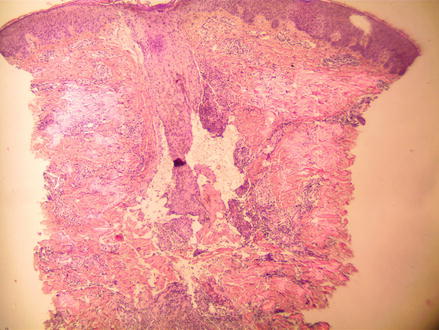
Figure 16.2
H&E 40×, central hair follicle is surrounded by mixed inflammation
The bacterial etiology of folliculitis can be divided into two groups, those caused by gram-positive bacteria and those caused by gram-negative bacteria. The majority of cases of bacterial folliculitis are caused by Staphylococcus aureus. In the past, methicillin–resistant Staphylococcus aureus (MRSA) was more likely to be present in the form of cellulitis. However, the incidence of MRSA folliculitis is on the rise. Fortunately, MRSA cellullitis and methicillin–sensitive Staphylococcus aureus (MSSA) folliculitis have clinically distinct presentations and this helps dermatologists in making the accurate diagnosis. MSSA folliculitis is still more common and tends to be found in the axillary region, beard, buttocks, and extremities of patients. In contrast, MRSA folliculitis appears in a more atypical distribution around the umbilicus, chest, flank, and scrotum.
Folliculitis caused by Staphylococcus is more likely to occur in patients who are immunocompromised, hyperhidrotic, atopic or who have a history of MRSA infections. Those individuals are likely to be chronic nasal Staphylococcus carriers and prone to recurrent infections. When Staphylococcus infects the hair follicles in the beard region, it is referred to as sycosis barbae. If it affects the posterior neck, it is called sycosis nuchae.
Gram-negative rods make up the second group of bacteria that can cause folliculitis. This collection of bacteria includes the Klebsiella, Escherichia coli, Proteus, and Enterobacter species. Follicular infection by gram-negative bacteria is less common than infection from S. aureus. However, cases of gram-negative bacteria tend to be more recalcitrant and difficult to eradicate. Most cases of gram-negative folliculitis are secondary to long-term use of oral tetracyclines for acne treatment.
Another gram-negative microbe that causes folliculitis is Pseudomonas aeruginosa. Also referred to as “hot tub folliculitis” P. aeruginosa is responsible for the acute onset of folliculitis 12–48 h after the use of a contaminated hot tub. These lesions tend to be more edematous in appearance. A study published by Lutz and Lee demonstrated the recent increase in multi-drug resistant P. aeruginosa. The study showed that 96 % of the P. aeruginosa organisms taken from swimming pools and hot tubs exhibited multi-drug resistance.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








