Fig. 1
Pre-operative anteroposterior (a), lateral (b), and Saltzman (c) view radiographs. On the AP view, note the radiolucent change that is present around the rod. On the lateral view, note the radiolucency around the posterior-to-anterior screw. On the Saltzman view, note the complete lateral disassociation of the hindfoot with respect to the tibia (Copyright 2014, Rubin Institute for Advanced Orthopedics, Sinai Hospital of Baltimore)
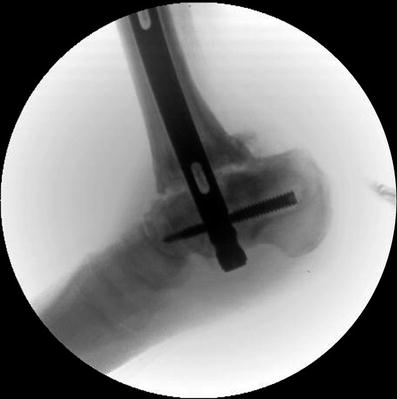
Fig. 2
Pre-operative lateral view fluoroscopic image (Copyright 2014, Rubin Institute for Advanced Orthopedics, Sinai Hospital of Baltimore)

Fig. 3
Photo shows short right extremity and patient’s “kickstand” right foot (Copyright 2014, Rubin Institute for Advanced Orthopedics, Sinai Hospital of Baltimore)
3 Preoperative Problem List
Nonunion
Infection
LLD
4 Treatment Strategy
Our strategy was to perform minimally invasive surgery to correct alignment and LLD. The intramedullary rod was removed, and the intramedullary canal was thoroughly irrigated and debrided. The nonunion site was not opened. The external fixator was then applied in order to gradually correct the deformity and LLD through the nonunion site. She received oral antibioics after this surgery. Distraction was performed at a rate of 0.5 mm per day. The patient was allowed weight-bearing as tolerated and completed the distraction phase of treatment 1 month after application of the TSF. After the distraction phase, she used an external bone stimulator to promote union. Distraction osteogenesis of a hypertrophic nonunion is effective for promoting bony union while at the same time correcting the LLD and the deformity. She had a minor pin tract infection that was treated with oral antibiotics. The chronic infection that she presented with did not seem to be clinically relevant. After the external fixation was removed, a short leg cast (non-weight-bearing status) was applied to protect the open pin sites. The short leg cast remained in place for 2 weeks, and then, a walking cast was applied for 6 weeks. Then, the patient transitioned to a custom ankle foot orthosis (AFO) with weight-bearing as tolerated. At 1-year follow-up, she did not use the AFO. She wore a shoe lift as well as a rocker bottom shoe to allow for ambulation. Radiographs obtained 1 year after removal showed progressive bony healing at the fusion site; therefore, no additional measures were taken to augment bone healing.









