Procedure 5 Surgical Treatment of Trigger Digits
![]() See Video 2: Surgical Treatment of Trigger Digits
See Video 2: Surgical Treatment of Trigger Digits
Indications
 Failure of tendon sheath steroid injections
Failure of tendon sheath steroid injections
 A fixed flexion contracture of the proximal interphalangeal (PIP) joint owing to the triggering
A fixed flexion contracture of the proximal interphalangeal (PIP) joint owing to the triggering
 Trigger digits in patients with rheumatoid arthritis
Trigger digits in patients with rheumatoid arthritis
Examination/Imaging
Clinical Examination
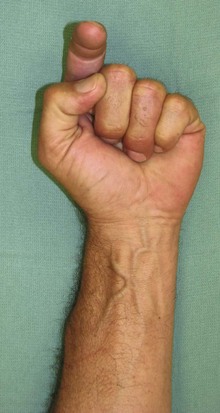
 The patient is examined for a palpable nodule at the level of A1 pulley. The patient may be unable to flex the finger or experience a catching when the finger flexes as the enlarged tendon passes through the A1 pulley (Fig. 5-1).
The patient is examined for a palpable nodule at the level of A1 pulley. The patient may be unable to flex the finger or experience a catching when the finger flexes as the enlarged tendon passes through the A1 pulley (Fig. 5-1).
 The grade of triggering should be recorded for follow-up purposes (Table 5-1). One should look for tenderness over the A1 pulley and a palpable nodule. In long-standing triggering, a flexion contracture of the PIP joint may be present, and the degree of contracture should be noted.
The grade of triggering should be recorded for follow-up purposes (Table 5-1). One should look for tenderness over the A1 pulley and a palpable nodule. In long-standing triggering, a flexion contracture of the PIP joint may be present, and the degree of contracture should be noted.
 The most frequently involved digit is the ring finger, followed by the thumb and the long, small, and index fingers. Patients who present with primary index finger trigger must be evaluated for associated conditions like diabetes and rheumatoid arthritis.
The most frequently involved digit is the ring finger, followed by the thumb and the long, small, and index fingers. Patients who present with primary index finger trigger must be evaluated for associated conditions like diabetes and rheumatoid arthritis.
 In patients with rheumatoid arthritis, one must carefully differentiate between the snapping observed in fingers with early swan-neck deformity and the catching seen in trigger finger. The snapping finger is due to the sudden return of the lateral bands from a dorsal to a palmar location over the condyle of the proximal phalanx as the patient actively corrects the hyperextension deformity. Occasionally triggering may be due to flexor tendon nodules getting caught under the carpal tunnel.
In patients with rheumatoid arthritis, one must carefully differentiate between the snapping observed in fingers with early swan-neck deformity and the catching seen in trigger finger. The snapping finger is due to the sudden return of the lateral bands from a dorsal to a palmar location over the condyle of the proximal phalanx as the patient actively corrects the hyperextension deformity. Occasionally triggering may be due to flexor tendon nodules getting caught under the carpal tunnel.
 Rarely, a locked metacarpophalangeal (MCP) joint can be confused with a trigger finger. A trigger finger primarily affects the interphalangeal joints and is usually gradual in onset, in contrast to the sudden onset of MCP joint locking. MCP joint locking usually results from collateral ligament injury, sesamoid, or osteophyte entrapment.
Rarely, a locked metacarpophalangeal (MCP) joint can be confused with a trigger finger. A trigger finger primarily affects the interphalangeal joints and is usually gradual in onset, in contrast to the sudden onset of MCP joint locking. MCP joint locking usually results from collateral ligament injury, sesamoid, or osteophyte entrapment.
 Congenital trigger thumb most commonly presents with a fixed flexion deformity, and less commonly with triggering. A characteristic nodule (Notta node) can be palpated on the flexor pollicis longus (FPL) tendon at the region of the A1 pulley. This can help differentiate congenital trigger thumb from other clasped thumb deformities.
Congenital trigger thumb most commonly presents with a fixed flexion deformity, and less commonly with triggering. A characteristic nodule (Notta node) can be palpated on the flexor pollicis longus (FPL) tendon at the region of the A1 pulley. This can help differentiate congenital trigger thumb from other clasped thumb deformities.
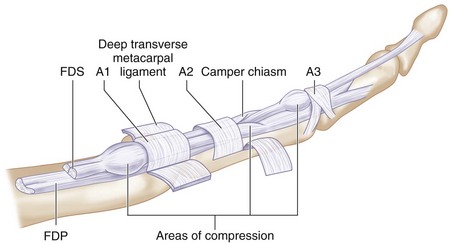
 Congenital trigger finger is a distinct entity related to abnormal thickening of the flexor digitorum superficialis (FDS) and flexor digitorum profundus (FDP), calcifications or granulations within the tendons, or abnormal relationship of the tendons at the FDS decussation. The common sites for triggering in a congenital trigger finger are the A1 pulley, the FDS chiasm, and the A3 pulley (Fig. 5-2).
Congenital trigger finger is a distinct entity related to abnormal thickening of the flexor digitorum superficialis (FDS) and flexor digitorum profundus (FDP), calcifications or granulations within the tendons, or abnormal relationship of the tendons at the FDS decussation. The common sites for triggering in a congenital trigger finger are the A1 pulley, the FDS chiasm, and the A3 pulley (Fig. 5-2).
Table 5-1 Grading of Trigger Digits
| Grade I | Before triggering | History of triggering, but not demonstrable on examination |
| Grade II | Active | Demonstrable triggering, but patient can actively overcome the trigger |
| Grade III | Passive | Demonstrable triggering, but patient cannot actively overcome trigger |
| • IIIA | • Extension | • Locked in flexion and needs passive extension to overcome trigger |
| • IIIB | • Flexion | • Locked in extension and needs passive flexion to overcome trigger |
| Grade IV | Contracture | Demonstrable trigger with flexion contracture of posterior interphalangeal joint |