Procedure 47 Lateral Arm Flap for Upper Limb Coverage
Indications
 Procedure is used for soft tissue defects of the hand and wrist. These defects range from a medium size of 3 × 5 cm to a large size of 15 × 20 cm and can include the following:
Procedure is used for soft tissue defects of the hand and wrist. These defects range from a medium size of 3 × 5 cm to a large size of 15 × 20 cm and can include the following:
 These skin defects are from loss of the full thickness of the dermis and the entire thickness of the subcutaneous tissues. The deeper tendons and neurovascular bundle could also be lacerated or could have suffered a segmental loss. The underlying bone could also be fractured. These defects include the following:
These skin defects are from loss of the full thickness of the dermis and the entire thickness of the subcutaneous tissues. The deeper tendons and neurovascular bundle could also be lacerated or could have suffered a segmental loss. The underlying bone could also be fractured. These defects include the following:
 Location of these soft tissue defects could be further classified as follows:
Location of these soft tissue defects could be further classified as follows:
 Free-flap version of the lateral arm flap is always preferred for the resurfacing. The flap is usually harvested from the ipsilateral side. The pedicled version of the flap is harvested from the contralateral side. The pedicled flap is chosen for the following indications:
Free-flap version of the lateral arm flap is always preferred for the resurfacing. The flap is usually harvested from the ipsilateral side. The pedicled version of the flap is harvested from the contralateral side. The pedicled flap is chosen for the following indications:
Examination/Imaging
Clinical Examination
 Preliminary assessment can be done with inspection of the wound and viewing of the clinical pictures previously taken of the defect. The definitive assessment is performed intraoperatively under anesthesia.
Preliminary assessment can be done with inspection of the wound and viewing of the clinical pictures previously taken of the defect. The definitive assessment is performed intraoperatively under anesthesia.
 The recipient defect is assessed to determine the reconstructive requirements.
The recipient defect is assessed to determine the reconstructive requirements.
 Assessing the availability of the recipient vessels
Assessing the availability of the recipient vessels
Surgical Anatomy
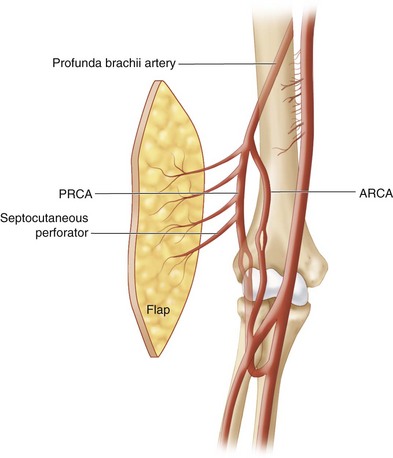
 The flap is from the lateral arm region with extension distal to the lateral humeral epicondyle down the lateral side of the forearm. The vascular pedicle is the posterior radial collateral artery (PRCA), a branch of the profunda brachii artery. One to two veins accompany the PRCA artery. The size of the artery is 1.5 to 2 mm in diameter, and the vein 2 to 3 mm in diameter. The vascular pedicle runs in the lateral intermuscular septum accompanied by the posterior antebrachial cutaneous nerve. Three to four septocutaneous perforators supply the lateral arm skin. The most distal branch of the septal vessel is 3 to 5 cm proximal to the lateral epicondyle. There are also three to four small branches of vessels running deep providing periosteal blood supply to the distal lateral humeral bone. The pedicle length of the flap ranges from 5 to 10 cm depending on the design of the flap (Fig. 47-3).
The flap is from the lateral arm region with extension distal to the lateral humeral epicondyle down the lateral side of the forearm. The vascular pedicle is the posterior radial collateral artery (PRCA), a branch of the profunda brachii artery. One to two veins accompany the PRCA artery. The size of the artery is 1.5 to 2 mm in diameter, and the vein 2 to 3 mm in diameter. The vascular pedicle runs in the lateral intermuscular septum accompanied by the posterior antebrachial cutaneous nerve. Three to four septocutaneous perforators supply the lateral arm skin. The most distal branch of the septal vessel is 3 to 5 cm proximal to the lateral epicondyle. There are also three to four small branches of vessels running deep providing periosteal blood supply to the distal lateral humeral bone. The pedicle length of the flap ranges from 5 to 10 cm depending on the design of the flap (Fig. 47-3).
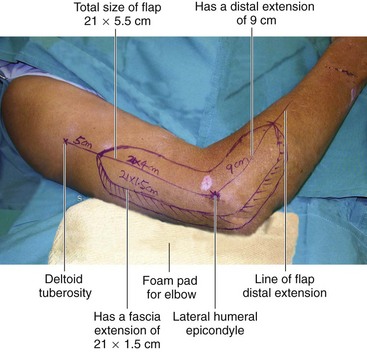
 The flap extends from the deltoid tuberosity to the lateral humeral epicondyle, a length of about 20 cm. The flap can be further extended distally down the lateral aspect of the forearm another 15 cm. The skin over the lateral forearm is thinner than the skin over the lateral arm. The width of the skin flap is limited to 6 cm to allow direct closure of the donor site. Centering the flap over the lateral humeral epicondyle has the advantage of having the thinner distal skin and a longer vascular pedicle.
The flap extends from the deltoid tuberosity to the lateral humeral epicondyle, a length of about 20 cm. The flap can be further extended distally down the lateral aspect of the forearm another 15 cm. The skin over the lateral forearm is thinner than the skin over the lateral arm. The width of the skin flap is limited to 6 cm to allow direct closure of the donor site. Centering the flap over the lateral humeral epicondyle has the advantage of having the thinner distal skin and a longer vascular pedicle.
 In a free-flap version, the ipsilateral flap is preferred. This gives the advantage of confining the wound to the same upper limb. In a pedicled flap version, the flap has to come from the contralateral arm.
In a free-flap version, the ipsilateral flap is preferred. This gives the advantage of confining the wound to the same upper limb. In a pedicled flap version, the flap has to come from the contralateral arm.
Positioning
 The patient is positioned supine with the hand and whole upper limb placed on a hand table.
The patient is positioned supine with the hand and whole upper limb placed on a hand table.
 The whole upper limb, including the shoulder, is prepared.
The whole upper limb, including the shoulder, is prepared.
 A sterile pressure tourniquet is applied to the arm as proximally as possible.
A sterile pressure tourniquet is applied to the arm as proximally as possible.
 A foam pad is used to cushion the elbow, taking pressure off the cubital tunnel and its ulnar nerve. (Fig. 47-4 shows design of 21 × 5.5 cm long and narrow flap design, with fascia extension.)
A foam pad is used to cushion the elbow, taking pressure off the cubital tunnel and its ulnar nerve. (Fig. 47-4 shows design of 21 × 5.5 cm long and narrow flap design, with fascia extension.)
 For a contralateral pedicled flap, both upper limbs are similarly prepared. The injured hand is brought across the chest to ensure its comfortable reach to the opposite arm.
For a contralateral pedicled flap, both upper limbs are similarly prepared. The injured hand is brought across the chest to ensure its comfortable reach to the opposite arm.
Pearls
In patients with a shorter arm, the sterile pressure tourniquet may occupy too much space, making proximal dissection difficult. A narrow manual rubber tourniquet of about 4 cm width can be used in its place effectively. However, the pressure cannot be regulated and is used only for a short duration for the proximal part of the dissection.
Flexion at the elbow and alternatively internal and external rotation at the shoulder facilitate greater reach in dissection of the flap.
Preparation of the Recipient Site
 Further débridement may be necessary.
Further débridement may be necessary.
 Skeletal fixation, repair, or grafting of deeper tissues is carried out if necessary.
Skeletal fixation, repair, or grafting of deeper tissues is carried out if necessary.
 Assessment of the skin defect and crafting a template is carried out.
Assessment of the skin defect and crafting a template is carried out.
 Exposure, preparation, and assessment of the recipient vessels are undertaken.
Exposure, preparation, and assessment of the recipient vessels are undertaken.