Figure 12.1
H&E 40×, ORF
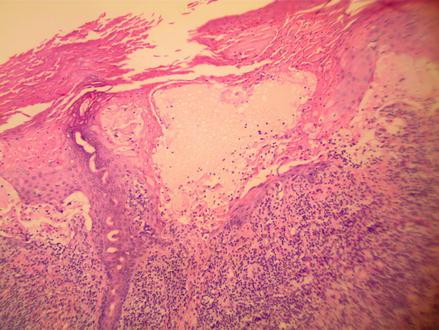
Figure 12.2
H&E 100×, ORF
There are reported cases of Orf infection triggering erythema multiforme, secondary bacterial infections, generalized papular or morbilliform reactions, as well as blistering eruptions similar to bullous pemphigoid in affected individuals. Some studies are arguing that these bullous eruptions observed after Orf infections are distinct autoimmune diseases.
The diagnosis is usually made based on history and physical examination. If a more thorough work up is required, electron microscopy may be performed on a scraping of the lesion. Also, a biopsy or polymerase chain reaction for viral RNA can be diagnostic. A herpes infection can identified by finding keratinocytes with multiple nuclei molded together. An irritant contact dermatitis can be elicited from the clinical history and extensive necrosis with neutrophils.
Treatment Options
Orf is typically a self-limiting infection that requires only supportive care. Most cases resolve completely within 2–7 weeks. Treatment only becomes necessary if secondary bacterial infection occurs or if the patient is immunocompromised.
Surgery and cryotherapy may be used to help debulk the infected tissue. There are also reports of using idoxuridine and cidofovir for either shortening healing time or help clear persistent infections. Other more recent therapies that could be considered include imiquimod cream and interferon.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








