Procedure 46 Pedicled Groin Flap
Indications
 Dorsal or palmar soft tissue defect of the hand (Fig. 46-1)
Dorsal or palmar soft tissue defect of the hand (Fig. 46-1)
 In preparation for a toe-to-thumb transfer following traumatic thumb or finger loss
In preparation for a toe-to-thumb transfer following traumatic thumb or finger loss
 Dorsal or palmar soft tissue defects involving multiple fingers
Dorsal or palmar soft tissue defects involving multiple fingers
 Circumferential thumb soft tissue defect
Circumferential thumb soft tissue defect
Examination/Imaging
Clinical Examination
 Patients should be examined for signs of previous surgery in the groin, including hernia repair, lymph node biopsy, or vein stripping. A higher incidence of thromboembolic and other general complications has been reported in patients older than 50 years with a pedicled groin flap, and an alternative method of coverage may be more suitable in older patients (e.g., a radial forearm flap), provided that the palmar arch is intact and there is no peripheral vascular disease affecting the circulation in the hand.
Patients should be examined for signs of previous surgery in the groin, including hernia repair, lymph node biopsy, or vein stripping. A higher incidence of thromboembolic and other general complications has been reported in patients older than 50 years with a pedicled groin flap, and an alternative method of coverage may be more suitable in older patients (e.g., a radial forearm flap), provided that the palmar arch is intact and there is no peripheral vascular disease affecting the circulation in the hand.
 The amount of skin required for thumb reconstruction is often underestimated, and the thickness of the flap increases the requirements when circumferential coverage is needed. A rough guideline with regard to the skin requirements in an adult male is as follows:
The amount of skin required for thumb reconstruction is often underestimated, and the thickness of the flap increases the requirements when circumferential coverage is needed. A rough guideline with regard to the skin requirements in an adult male is as follows:
 Morbidity: This flap requires attachment of the hand to the groin for 3 to 4 weeks, which restricts movements at all joints of the involved upper limb. Patients typically are able to shrug the shoulder, move the elbow minimally, and move the wrist and hand to a greater degree. This period of immobilization will result in stiffness, especially in older patients. In addition, patients will have the use of only one hand and may require help to manage toileting and other activities of daily living. There is a risk for injury to the lateral femoral cutaneous nerve with resultant loss of sensation in the lateral aspect of the thigh and, rarely, a painful neuroma. Patients need a minimum of two surgical procedures (one for inset and another for flap division) and occasionally may need more procedures (for flap delay and flap thinning). Patients must be informed about these issues before surgery.
Morbidity: This flap requires attachment of the hand to the groin for 3 to 4 weeks, which restricts movements at all joints of the involved upper limb. Patients typically are able to shrug the shoulder, move the elbow minimally, and move the wrist and hand to a greater degree. This period of immobilization will result in stiffness, especially in older patients. In addition, patients will have the use of only one hand and may require help to manage toileting and other activities of daily living. There is a risk for injury to the lateral femoral cutaneous nerve with resultant loss of sensation in the lateral aspect of the thigh and, rarely, a painful neuroma. Patients need a minimum of two surgical procedures (one for inset and another for flap division) and occasionally may need more procedures (for flap delay and flap thinning). Patients must be informed about these issues before surgery.
Surgical Anatomy
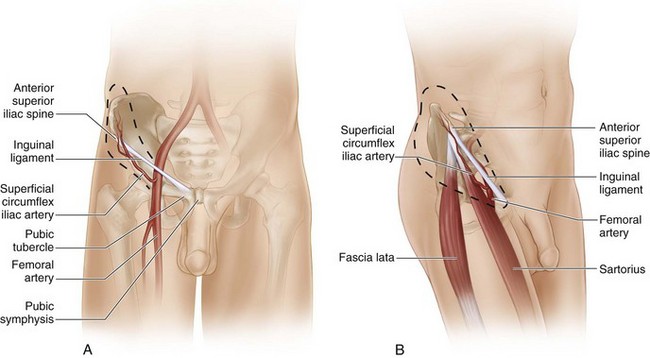
 Vascular basis: The flap is based on the superficial circumflex iliac artery (SCIA). The SCIA is the smallest branch of the femoral artery and arises about 1 inch below the inguinal ligament. It arises directly from the femoral artery in about 70% of cases; in the remainder, a common trunk is shared with the superficial epigastric artery. The SCIA travels obliquely toward the anterior superior iliac spine (ASIS), becoming progressively superficial as it travels from medial to lateral (Fig. 46-2A and B). At the medial border of the sartorius, the SCIA divides into a deep branch (which remains below the deep fascia and enters the sartorius) and a superficial branch (which pierces the deep fascia, becomes superficial, and supplies the overlying skin on its way to the ASIS). The femoral artery can be palpated immediately below the inguinal ligament at the midinguinal point (midway between pubic symphysis and ASIS). A point is marked 1 inch (2 fingerbreadths) below the inguinal ligament along the femoral artery. This represents the origin of the SCIA. A line drawn from this point to the ASIS represents the course of the SCIA and the vascular axis of the flap. Because of the obliquity of the vascular axis, about two thirds of the flap is designed superior to this axis and one third below this axis.
Vascular basis: The flap is based on the superficial circumflex iliac artery (SCIA). The SCIA is the smallest branch of the femoral artery and arises about 1 inch below the inguinal ligament. It arises directly from the femoral artery in about 70% of cases; in the remainder, a common trunk is shared with the superficial epigastric artery. The SCIA travels obliquely toward the anterior superior iliac spine (ASIS), becoming progressively superficial as it travels from medial to lateral (Fig. 46-2A and B). At the medial border of the sartorius, the SCIA divides into a deep branch (which remains below the deep fascia and enters the sartorius) and a superficial branch (which pierces the deep fascia, becomes superficial, and supplies the overlying skin on its way to the ASIS). The femoral artery can be palpated immediately below the inguinal ligament at the midinguinal point (midway between pubic symphysis and ASIS). A point is marked 1 inch (2 fingerbreadths) below the inguinal ligament along the femoral artery. This represents the origin of the SCIA. A line drawn from this point to the ASIS represents the course of the SCIA and the vascular axis of the flap. Because of the obliquity of the vascular axis, about two thirds of the flap is designed superior to this axis and one third below this axis.
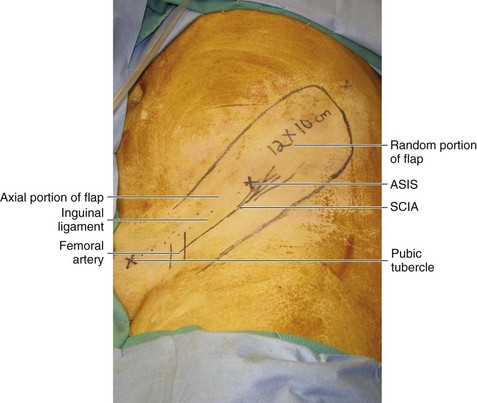
 Flap size: The maximum size of a groin flap is about 13 × 10 cm. This is adequate to resurface most soft tissue defects of the hand and thumb. However, this will not allow tubing of the flap in most cases without further medial dissection (Fig. 46-3).
Flap size: The maximum size of a groin flap is about 13 × 10 cm. This is adequate to resurface most soft tissue defects of the hand and thumb. However, this will not allow tubing of the flap in most cases without further medial dissection (Fig. 46-3).