Procedure 41 Centralization for Radial Longitudinal Deficiency
![]() See Video 34: Centralization for Radial Deficiency
See Video 34: Centralization for Radial Deficiency
Indications
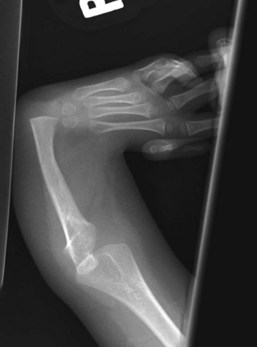
 Radial longitudinal deficiency (RLD) has been classified into four grades depending on the degree of hypoplasia of the radius (Table 41-1). Centralization is usually performed at 9 to 12 months of age because anesthesia is safer, preliminary soft tissue distraction can be carried out, and subsequent thumb reconstruction can be done before the child develops a maladaptive pattern.
Radial longitudinal deficiency (RLD) has been classified into four grades depending on the degree of hypoplasia of the radius (Table 41-1). Centralization is usually performed at 9 to 12 months of age because anesthesia is safer, preliminary soft tissue distraction can be carried out, and subsequent thumb reconstruction can be done before the child develops a maladaptive pattern.
 This procedure may be done first for children with type 0 or 1 deficiencies.
This procedure may be done first for children with type 0 or 1 deficiencies.
 Children with type 2 or greater deficiencies may need preliminary serial casting or soft tissue distraction using an external fixator.
Children with type 2 or greater deficiencies may need preliminary serial casting or soft tissue distraction using an external fixator.
Table 41-1 Classification of Radial Longitudinal Deficiency
| Type | Distal Radius | Proximal Radius |
|---|---|---|
| N | Normal | Normal |
| 0 | Normal | Normal, radioulnar synostosis, congenital radial head dislocation |
| 1 | >2 mm shorter than ulna | Normal, radioulnar synostosis, congenital radial head dislocation |
| 2 | Hypoplasia | Hypoplasia |
| 3 | Physis absent | Variable hypoplasia |
| 4 | Absent | Absent |
Examination/Imaging
Clinical Examination
 Sixty percent to 70% of children with RLD have an associated systemic or musculoskeletal abnormality, the most common being scoliosis. Therefore, before surgery, all children with RLD should undergo a thorough musculoskeletal and systemic examination, including spinal radiographs, cardiac echocardiographic evaluation, renal ultrasound, and a complete blood count.
Sixty percent to 70% of children with RLD have an associated systemic or musculoskeletal abnormality, the most common being scoliosis. Therefore, before surgery, all children with RLD should undergo a thorough musculoskeletal and systemic examination, including spinal radiographs, cardiac echocardiographic evaluation, renal ultrasound, and a complete blood count.
 It is important to assess elbow function. Some children are unable to flex the elbow, and the radial deviation deformity allows them to get the hand to the mouth. Correction of the radial deformity may improve the appearance but will limit function.
It is important to assess elbow function. Some children are unable to flex the elbow, and the radial deviation deformity allows them to get the hand to the mouth. Correction of the radial deformity may improve the appearance but will limit function.
Surgical Anatomy
 Children with RLD have anomalies involving the muscular, vascular, and nervous systems in addition to the obvious skeletal deformity.
Children with RLD have anomalies involving the muscular, vascular, and nervous systems in addition to the obvious skeletal deformity.
 Skeletal anomalies: The radius is either absent or partially developed, and the ulna is bowed posteriorly and shortened to two thirds its normal length. The articulation between the carpus and ulna does not form a normal joint. It is usually fibrous but can be lined by hyaline cartilage.
Skeletal anomalies: The radius is either absent or partially developed, and the ulna is bowed posteriorly and shortened to two thirds its normal length. The articulation between the carpus and ulna does not form a normal joint. It is usually fibrous but can be lined by hyaline cartilage.
 Muscle anomalies: The extensor carpi radialis longus and brevis may be absent or fused to the extensor digitorum communis (EDC). The extensor pollicis longus (EPL), extensor pollicis brevis (EPB), and abductor pollicis longus (APL) are present if the thumb metacarpal is present, or they may be fused to the surrounding tissues. The supinator is generally absent, as is the pronator quadratus. The pronator teres is absent if the radius is absent. The flexor carpi radialis longus and brevis are often absent. The flexor carpi ulnaris is usually present and normal, as is the flexor digitorum superficialis. The palmaris longus is often absent. The flexor pollicis longus is present only if the thumb metacarpal is present. If the thumb is present, the thenar muscles are usually present. The hypothenar, interosseous, and lumbrical muscles are usually normal.
Muscle anomalies: The extensor carpi radialis longus and brevis may be absent or fused to the extensor digitorum communis (EDC). The extensor pollicis longus (EPL), extensor pollicis brevis (EPB), and abductor pollicis longus (APL) are present if the thumb metacarpal is present, or they may be fused to the surrounding tissues. The supinator is generally absent, as is the pronator quadratus. The pronator teres is absent if the radius is absent. The flexor carpi radialis longus and brevis are often absent. The flexor carpi ulnaris is usually present and normal, as is the flexor digitorum superficialis. The palmaris longus is often absent. The flexor pollicis longus is present only if the thumb metacarpal is present. If the thumb is present, the thenar muscles are usually present. The hypothenar, interosseous, and lumbrical muscles are usually normal.
 Vascular anomalies: The brachial and ulnar artery are usually present and normal, but the radial artery is absent or attenuated. The interosseous arteries are usually well developed.
Vascular anomalies: The brachial and ulnar artery are usually present and normal, but the radial artery is absent or attenuated. The interosseous arteries are usually well developed.
 Nerve anomalies: The median and ulnar nerves are present, but the median nerve is the most superficial structure on the radial side of the arm and may be confused during surgical dissection with a tendinous structure. The median nerve must be identified first during the exposure. The radial nerve frequently ends at the elbow; thus, the median nerve supplies sensation to the radial side of the arm.
Nerve anomalies: The median and ulnar nerves are present, but the median nerve is the most superficial structure on the radial side of the arm and may be confused during surgical dissection with a tendinous structure. The median nerve must be identified first during the exposure. The radial nerve frequently ends at the elbow; thus, the median nerve supplies sensation to the radial side of the arm.