Procedure 39 Pollicization for Congenital Thumb Hypoplasia
Indications
 Hypoplastic thumb exists with inadequate carpometacarpal joint (Blauth types IIB, IV, and V).
Hypoplastic thumb exists with inadequate carpometacarpal joint (Blauth types IIB, IV, and V).
 Pollicization should be considered at about 12 to 18 months of age because at this age general anesthesia is safer and surgical dissection of critical structures is technically easier. In addition, this allows for preliminary correction of any associated radial deficiencies.
Pollicization should be considered at about 12 to 18 months of age because at this age general anesthesia is safer and surgical dissection of critical structures is technically easier. In addition, this allows for preliminary correction of any associated radial deficiencies.
Examination/Imaging
Clinical Examination
 The Blauth classification of thumb hypoplasia is useful in determining treatment options. Types IV (floating thumb) (Fig. 39-1) and V (absent thumb) (Fig. 39-2) are straightforward to identify clinically. However, it can be challenging to differentiate type IIIA (stable carpometacarpal [CMC] joint) from type IIIB (unstable CMC joint), and the trapezium and trapezoid are ossified only at 5 to 6 years of age, making radiographs less useful in decision making.
The Blauth classification of thumb hypoplasia is useful in determining treatment options. Types IV (floating thumb) (Fig. 39-1) and V (absent thumb) (Fig. 39-2) are straightforward to identify clinically. However, it can be challenging to differentiate type IIIA (stable carpometacarpal [CMC] joint) from type IIIB (unstable CMC joint), and the trapezium and trapezoid are ossified only at 5 to 6 years of age, making radiographs less useful in decision making.
 Serial examination of a child is required to differentiate between types IIIA and IIIB. A newborn uses digital grasp, and the infant begins to use the thumb in grasp at about 1 year of age. If the child uses the thumb in manipulating objects, this suggests that a type IIIA deficiency is present. If the child prefers to grasp objects between the index and long finger web space, this web appears wider, and the index finger is pronated toward the thumb. This suggests type IIIB hypoplasia.
Serial examination of a child is required to differentiate between types IIIA and IIIB. A newborn uses digital grasp, and the infant begins to use the thumb in grasp at about 1 year of age. If the child uses the thumb in manipulating objects, this suggests that a type IIIA deficiency is present. If the child prefers to grasp objects between the index and long finger web space, this web appears wider, and the index finger is pronated toward the thumb. This suggests type IIIB hypoplasia.
 The index finger may be stiff and hypoplastic to varying degrees in children with type IV and type V hypoplasia, which will affect the result of pollicization.
The index finger may be stiff and hypoplastic to varying degrees in children with type IV and type V hypoplasia, which will affect the result of pollicization.
 The child should be examined for signs of other systematic abnormalities, such as VACTERL (i.e., vertebral abnormalities, anal atresia, cardiac abnormalities, tracheoesophageal fistula and/or esophageal atresia, renal agenesis and dysplasia, and limb defects), Fanconi anemia, and Holt-Oltram syndrome, before considering surgical reconstruction.
The child should be examined for signs of other systematic abnormalities, such as VACTERL (i.e., vertebral abnormalities, anal atresia, cardiac abnormalities, tracheoesophageal fistula and/or esophageal atresia, renal agenesis and dysplasia, and limb defects), Fanconi anemia, and Holt-Oltram syndrome, before considering surgical reconstruction.
Imaging
 Radiographs of the hands, wrists, and forearms are useful in determining the degree of metacarpal and phalangeal hypoplasia of the thumb and index finger. They can also identify other associated upper extremity anomalies, such as radial deficiency.
Radiographs of the hands, wrists, and forearms are useful in determining the degree of metacarpal and phalangeal hypoplasia of the thumb and index finger. They can also identify other associated upper extremity anomalies, such as radial deficiency.
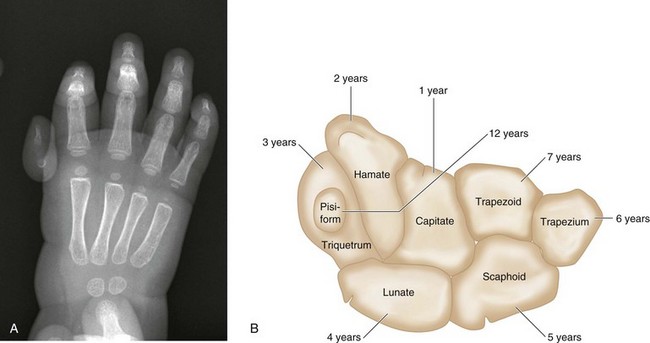
 The number of carpal bones seen on the radiograph gives a rough estimate of the age of the child (Fig. 39-3A). The order of ossification of carpal bones is detailed in Figure 39-3B. About one center appears per year from the age of 1 year to 7 years.
The number of carpal bones seen on the radiograph gives a rough estimate of the age of the child (Fig. 39-3A). The order of ossification of carpal bones is detailed in Figure 39-3B. About one center appears per year from the age of 1 year to 7 years.
 The presence of a tapered metacarpal without a base confirms type IIIB hypoplasia. Type IIIA hypoplasia is associated with full length of the metacarpal (Fig. 39-4).
The presence of a tapered metacarpal without a base confirms type IIIB hypoplasia. Type IIIA hypoplasia is associated with full length of the metacarpal (Fig. 39-4).
Surgical Anatomy
 After pollicization, the common digital artery to the index and long fingers is the primary blood supply to the transposed digit. The radial digital artery to the index finger may be absent, but the ability to perform index pollicization is not contingent on the presence of the radial digital artery when the main blood supply comes from the ulnar digital artery.
After pollicization, the common digital artery to the index and long fingers is the primary blood supply to the transposed digit. The radial digital artery to the index finger may be absent, but the ability to perform index pollicization is not contingent on the presence of the radial digital artery when the main blood supply comes from the ulnar digital artery.
Positioning
 The procedure is conducted under general anesthesia with the patient placed supine on the operating room table. The entire upper extremity is prepared and draped after a tourniquet is applied.
The procedure is conducted under general anesthesia with the patient placed supine on the operating room table. The entire upper extremity is prepared and draped after a tourniquet is applied.
 The limb is exsanguinated fully to permit a completely bloodless field. A well-fitted, small tourniquet is essential because blood in the operative field will jeopardize the operation by obscuring the small structures in the pediatric hand.
The limb is exsanguinated fully to permit a completely bloodless field. A well-fitted, small tourniquet is essential because blood in the operative field will jeopardize the operation by obscuring the small structures in the pediatric hand.
Exposures
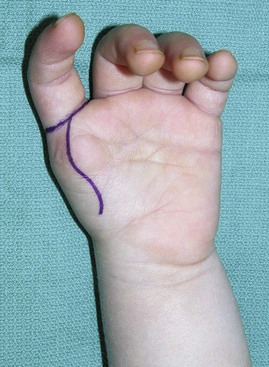
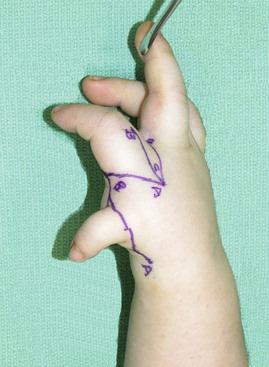
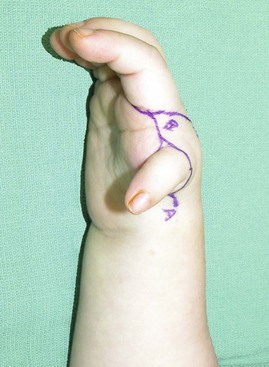
 A longitudinal curvilinear incision is marked over the palmar aspect of the index finger metacarpal (Fig. 39-5). A V-shaped incision is marked over the dorsum of the index finger metacarpal such that the apex is at the level of the neck of the metacarpal (Figs. 39-6 and 39-7). The dorsal and palmar incisions are connected at the base of the finger. A longitudinal incision is marked over the dorsum of the proximal phalanx, extending from the proximal interphalangeal (PIP) joint to the apex of the V.
A longitudinal curvilinear incision is marked over the palmar aspect of the index finger metacarpal (Fig. 39-5). A V-shaped incision is marked over the dorsum of the index finger metacarpal such that the apex is at the level of the neck of the metacarpal (Figs. 39-6 and 39-7). The dorsal and palmar incisions are connected at the base of the finger. A longitudinal incision is marked over the dorsum of the proximal phalanx, extending from the proximal interphalangeal (PIP) joint to the apex of the V.
Pearls
If the thumb is present, the hypoplastic digit may be filleted and the skin incorporated into the design of the skin flaps or into the first web space for additional soft tissue coverage (Figs. 39-8 and 39-9).