Procedure 38 Reconstruction for Congenital Thumb Hypoplasia
Congenital thumb hypoplasia can vary from mild size discrepancy to complete absence. The Blauth classification is useful for categorizing the degree of development (Table 38-1). It is critical to assess the stability of the thumb carpometacarpal (CMC) joint to determine the appropriate surgical treatment for thumb hypoplasia. The goal of surgical intervention for children with a stable CMC joint (Blauth types I, II, and IIIA) is preservation of the existing thumb and augmentation of the deficient soft tissue elements. Conversely, if the CMC joint is unstable or absent (Blauth types IIIB, IV, and V), any remnants of the existing thumb should be ablated, and reconstruction should proceed by pollicizing the index finger. This chapter focuses on the reconstruction of Blauth types I, II, and IIIA hypoplasia.
Table 38-1 Blauth Classification of Thumb Hypoplasia and Treatment Options
| Type | Features | Treatment Options |
|---|---|---|
| I | Mild hypoplasia with all elements present | No treatment |
| II | Narrow first web, ulnar collateral ligament insufficiency, and absence of thenar intrinsic muscles | No treatment Z-plasty of first web, UCL strengthening/reconstruction, and opponensplasty |
| III | Type II plus extrinsic tendon deficiencies and/or skeletal deficiency | |
| IIIA | Stable CMC joint | Same as type II |
| IIIB | Unstable CMC joint | Pollicization |
| IV | Absent metacarpal and rudimentary phalanges “Pouce flottant” | Pollicization |
| V | Total absence | Pollicization |
Indications
 Congenital thumb hypoplasia is seen with a stable CMC joint with varying degrees of soft tissue deficiency (Blauth types I, II, and IIIA). The important soft tissue deficiencies are the following:
Congenital thumb hypoplasia is seen with a stable CMC joint with varying degrees of soft tissue deficiency (Blauth types I, II, and IIIA). The important soft tissue deficiencies are the following:
 Reconstructive procedures for thumb hypoplasia (Blauth types I, II, and IIIA) can be performed at a later age (2 to 4 years) because the child can use the thumb for activities without developing maladaptive compensation patterns. However, it is preferable to correct these deformities before the child enters school to avoid any stigma from an uncorrected deformity.
Reconstructive procedures for thumb hypoplasia (Blauth types I, II, and IIIA) can be performed at a later age (2 to 4 years) because the child can use the thumb for activities without developing maladaptive compensation patterns. However, it is preferable to correct these deformities before the child enters school to avoid any stigma from an uncorrected deformity.
Examination/Imaging
Clinical Examination
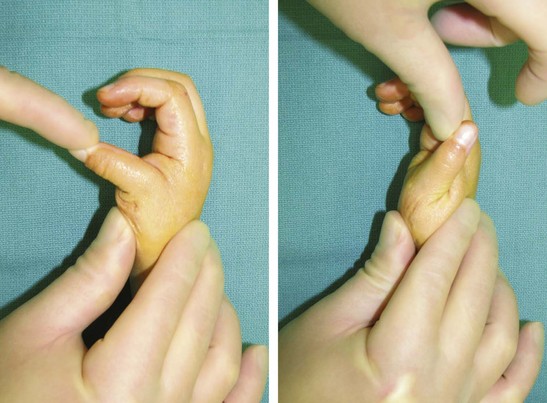
 The child should be examined to assess the degree of first web narrowing, opposition function of the thumb, and stability of the thumb MCP joint (Fig. 38-1). Serial examination of a child is required to differentiate between Blauth types IIIA and IIIB. A newborn child uses digital grasp and begins to use the thumb in grasp at about 1 year of age. If the child uses the thumb in manipulating objects, this suggests that a type IIIA deficiency is present. If the child prefers to grasp objects between the index and long finger web space, this web space appears wider because the index finger is pronated toward the thumb. This suggests type IIIB hypoplasia because the child is incapable of using the unstable thumb for effective pinch.
The child should be examined to assess the degree of first web narrowing, opposition function of the thumb, and stability of the thumb MCP joint (Fig. 38-1). Serial examination of a child is required to differentiate between Blauth types IIIA and IIIB. A newborn child uses digital grasp and begins to use the thumb in grasp at about 1 year of age. If the child uses the thumb in manipulating objects, this suggests that a type IIIA deficiency is present. If the child prefers to grasp objects between the index and long finger web space, this web space appears wider because the index finger is pronated toward the thumb. This suggests type IIIB hypoplasia because the child is incapable of using the unstable thumb for effective pinch.
 The entire upper extremity should be examined for other elements of radial deficiency, and patients should be examined for systemic manifestations of associated hematologic and cardiac syndromes such as Holt-Oram, thrombocytopenia-absent-radius (TAR) syndrome, VACTERL (i.e., vertebral abnormalities, anal atresia, cardiac abnormalities, tracheoesophageal fistula and/or esophageal atresia, renal agenesis and dysplasia, and limb defects), and Fanconi anemia.
The entire upper extremity should be examined for other elements of radial deficiency, and patients should be examined for systemic manifestations of associated hematologic and cardiac syndromes such as Holt-Oram, thrombocytopenia-absent-radius (TAR) syndrome, VACTERL (i.e., vertebral abnormalities, anal atresia, cardiac abnormalities, tracheoesophageal fistula and/or esophageal atresia, renal agenesis and dysplasia, and limb defects), and Fanconi anemia.
Surgical Anatomy
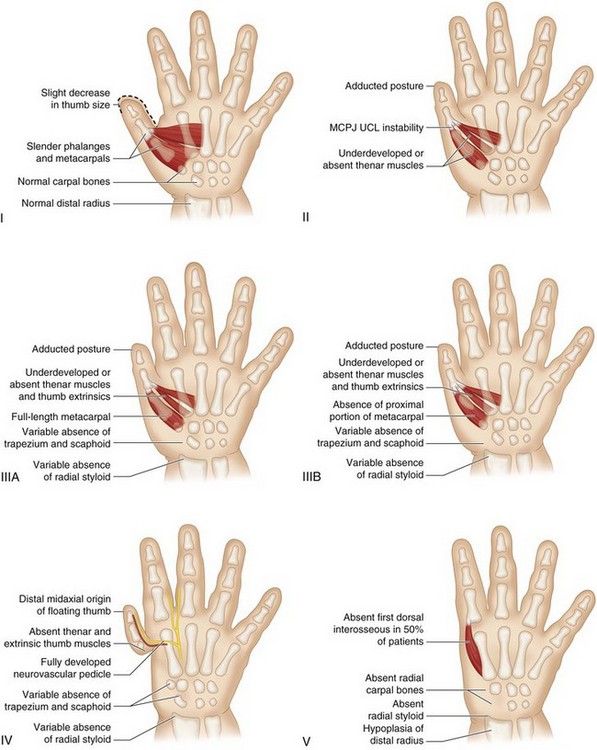
 The anatomic deficiencies associated with thumb hypoplasia are detailed in Figure 38-3. The ulnar collateral ligament spans the MCP joint of the thumb and is lax in type II and type III thumbs.
The anatomic deficiencies associated with thumb hypoplasia are detailed in Figure 38-3. The ulnar collateral ligament spans the MCP joint of the thumb and is lax in type II and type III thumbs.
 The intrinsic muscles of the thumb (abductor pollicis brevis [APB], opponens pollicis [OP], flexor pollicis brevis [FPB], and adductor pollicis [AP]) are deficient in types II and III and absent in types IV and V.
The intrinsic muscles of the thumb (abductor pollicis brevis [APB], opponens pollicis [OP], flexor pollicis brevis [FPB], and adductor pollicis [AP]) are deficient in types II and III and absent in types IV and V.
 The flexor pollicis longus (FPL) and extensor pollicis longus (EPL) are hypoplastic in type III thumbs. Often, there may be an anomalous connection between the FPL and the EPL at the level of the MCP joint, known as pollex abductus. This connection can attenuate the UCL over time and prevent active interphalangeal joint motion.
The flexor pollicis longus (FPL) and extensor pollicis longus (EPL) are hypoplastic in type III thumbs. Often, there may be an anomalous connection between the FPL and the EPL at the level of the MCP joint, known as pollex abductus. This connection can attenuate the UCL over time and prevent active interphalangeal joint motion.
Exposures
 The authors use a four-flap Z-plasty to widen the first web space and perform a transfer of the abductor digiti minimi (Huber transfer) for opponensplasty (Fig. 38-4), and a reefing combined with an adductor advancement for strengthening the UCL and stabilizing the MCP joint. All patients may not need all three procedures, and incisions should be planned appropriately.
The authors use a four-flap Z-plasty to widen the first web space and perform a transfer of the abductor digiti minimi (Huber transfer) for opponensplasty (Fig. 38-4), and a reefing combined with an adductor advancement for strengthening the UCL and stabilizing the MCP joint. All patients may not need all three procedures, and incisions should be planned appropriately.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree