Procedure 33 Correction of Swan-Neck Deformity in the Rheumatoid Hand
![]() See Video 25: Lateral Band Release for Rheumatoid Swan-Neck Deformity
See Video 25: Lateral Band Release for Rheumatoid Swan-Neck Deformity
Indications
 Treatment of swan-neck deformity is based on the flexibility of the proximal interphalangeal (PIP) joint and condition of the joint cartilage.
Treatment of swan-neck deformity is based on the flexibility of the proximal interphalangeal (PIP) joint and condition of the joint cartilage.
 The Nalebuff classification is the most widely accepted and useful method for surgical decision-making.
The Nalebuff classification is the most widely accepted and useful method for surgical decision-making.
 Type I deformities need a procedure to limit PIP hyperextension (e.g., splint, dermodesis, flexor digitorum superficialis [FDS] tenodesis) and restore distal interphalangeal (DIP) extension (e.g., tenodermodesis, fusion).
Type I deformities need a procedure to limit PIP hyperextension (e.g., splint, dermodesis, flexor digitorum superficialis [FDS] tenodesis) and restore distal interphalangeal (DIP) extension (e.g., tenodermodesis, fusion).
 Type II deformities require an intrinsic release and/or MCP joint arthroplasty in addition to the procedure for type I.
Type II deformities require an intrinsic release and/or MCP joint arthroplasty in addition to the procedure for type I.
 Type III deformities require restoration of flexion of the PIP joint by manipulation, lateral band mobilization, and lengthening of the central slip depending on the severity of soft tissue contracture.
Type III deformities require restoration of flexion of the PIP joint by manipulation, lateral band mobilization, and lengthening of the central slip depending on the severity of soft tissue contracture.
 Arthrodesis of the PIP joint is often recommended for type IV deformities with joint destruction; however, implant arthroplasty is always an option.
Arthrodesis of the PIP joint is often recommended for type IV deformities with joint destruction; however, implant arthroplasty is always an option.
Examination/Imaging
Clinical Examination
 Active and passive range of motion of the PIP joint is tested with the MCP joint in extension and flexion. This is to evaluate whether the intrinsic muscles are contributing to the restricted PIP joint motion. Restriction in radial and ulnar deviation is also tested with the MCP joint in extension to evaluate which of the intrinsic muscles is responsible for the PIP joint tightness.
Active and passive range of motion of the PIP joint is tested with the MCP joint in extension and flexion. This is to evaluate whether the intrinsic muscles are contributing to the restricted PIP joint motion. Restriction in radial and ulnar deviation is also tested with the MCP joint in extension to evaluate which of the intrinsic muscles is responsible for the PIP joint tightness.
 When active motion of the PIP is not nearly equal to passive motion, adhesions of the flexor tendons must be suspected.
When active motion of the PIP is not nearly equal to passive motion, adhesions of the flexor tendons must be suspected.
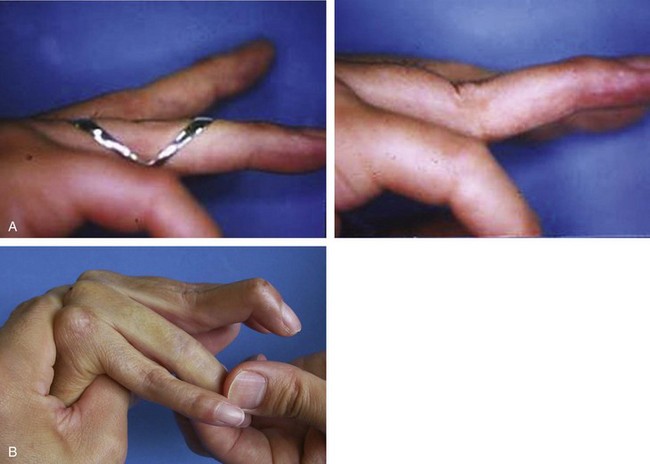
 When the PIP joint is flexible regardless of the metacarpophalangeal (MCP) joint position (type I), a PIP extension block splint may correct the deformity while restoring full flexion (Fig. 33-1A).
When the PIP joint is flexible regardless of the metacarpophalangeal (MCP) joint position (type I), a PIP extension block splint may correct the deformity while restoring full flexion (Fig. 33-1A).
 When flexion of the PIP joint is restricted with the MCP joint in extension and radial deviation, ulnar intrinsic muscle tightness exists.
When flexion of the PIP joint is restricted with the MCP joint in extension and radial deviation, ulnar intrinsic muscle tightness exists.
 When passive flexion of the PIP is limited with the MCP joint in flexion, the pathology is the stiff PIP joint (type III) (Fig. 33-1B).
When passive flexion of the PIP is limited with the MCP joint in flexion, the pathology is the stiff PIP joint (type III) (Fig. 33-1B).
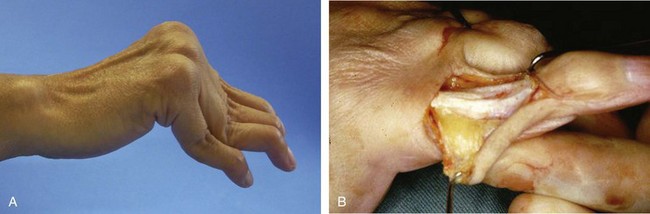
 The typical swan-neck deformity is associated with flexion contracture of the MCP joint, hyperextension of the PIP joints, and dorsally displaced lateral bands (Fig. 33-2).
The typical swan-neck deformity is associated with flexion contracture of the MCP joint, hyperextension of the PIP joints, and dorsally displaced lateral bands (Fig. 33-2).
Surgical Anatomy
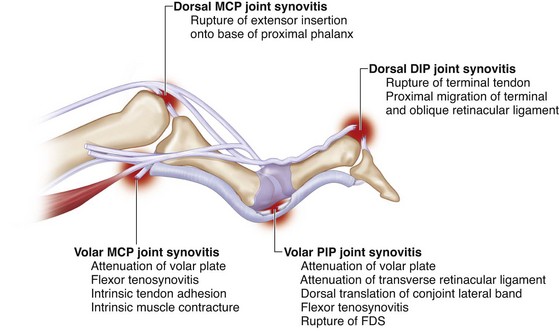
 A swan-neck deformity can occur as a result of abnormalities at the wrist, MCP joint, PIP joint, or DIP joint (Fig. 33-3).
A swan-neck deformity can occur as a result of abnormalities at the wrist, MCP joint, PIP joint, or DIP joint (Fig. 33-3).
 Synovitis within the PIP joint leads to stretching, weakening, and eventually destruction of the volar plate and collateral ligaments and the insertion of the FDS, resulting in the loss of palmar restraint at the PIP joint. This loss allows the normal extensor forces to cause abnormal hyperextension of the PIP joint.
Synovitis within the PIP joint leads to stretching, weakening, and eventually destruction of the volar plate and collateral ligaments and the insertion of the FDS, resulting in the loss of palmar restraint at the PIP joint. This loss allows the normal extensor forces to cause abnormal hyperextension of the PIP joint.
 Synovitis of the MCP joint causes attenuation of the volar plate, resulting in volar subluxation of the MCP joint. Over time, volar subluxation results in shortening of the intrinsic muscles, leading to PIP joint hyperextension and ultimately swan-neck deformity.
Synovitis of the MCP joint causes attenuation of the volar plate, resulting in volar subluxation of the MCP joint. Over time, volar subluxation results in shortening of the intrinsic muscles, leading to PIP joint hyperextension and ultimately swan-neck deformity.
 DIP joint synovitis can cause weakening and rupture of the terminal extensor tendon insertion, leading to the development of a mallet deformity. The proximal migration of the terminal extensor insertion causes the lateral bands to become lax. All the power of the common extrinsic extensor is now directed toward the central slip that inserts into the middle phalanx. Over time, the volar supporting structures of the PIP joint are weakened, and the PIP joint is forced into hyperextension, resulting in a swan-neck deformity.
DIP joint synovitis can cause weakening and rupture of the terminal extensor tendon insertion, leading to the development of a mallet deformity. The proximal migration of the terminal extensor insertion causes the lateral bands to become lax. All the power of the common extrinsic extensor is now directed toward the central slip that inserts into the middle phalanx. Over time, the volar supporting structures of the PIP joint are weakened, and the PIP joint is forced into hyperextension, resulting in a swan-neck deformity.
 Synovitis at the wrist joint can lead to carpal collapse, carpal supination, and ulnar translation. Carpal collapse leads to a relative lengthening (relaxation) of the long flexor and extensor tendons. The interosseous muscle can then overpower the action of the extrinsic muscles and lead to MCP joint flexion and PIP joint extension, which over a prolonged period causes a physiologic shortening of the intrinsic muscles.
Synovitis at the wrist joint can lead to carpal collapse, carpal supination, and ulnar translation. Carpal collapse leads to a relative lengthening (relaxation) of the long flexor and extensor tendons. The interosseous muscle can then overpower the action of the extrinsic muscles and lead to MCP joint flexion and PIP joint extension, which over a prolonged period causes a physiologic shortening of the intrinsic muscles.