Procedure 31 Tendon Transfers for Extensor and Flexor Tendon Ruptures
![]() See Video 23: Tendon Transfers for the Ruptured Flexor and Extensor Tendons
See Video 23: Tendon Transfers for the Ruptured Flexor and Extensor Tendons
Examination/Imaging
Clinical Examination
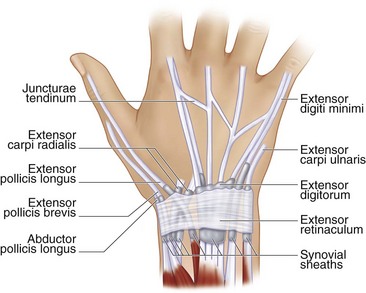
 The most frequently ruptured tendons in rheumatoid arthritis (RA) are the extensor digiti minimi (EDM), followed by the extensor digitorum communis (EDC) tendons to the small, ring, long, and index fingers, in that order; the extensor pollicis longus (EPL); the flexor pollicis longus (FPL); and, rarely, the flexor digitorum superficialis (FDS) and the flexor digitorum profundus (FDP).
The most frequently ruptured tendons in rheumatoid arthritis (RA) are the extensor digiti minimi (EDM), followed by the extensor digitorum communis (EDC) tendons to the small, ring, long, and index fingers, in that order; the extensor pollicis longus (EPL); the flexor pollicis longus (FPL); and, rarely, the flexor digitorum superficialis (FDS) and the flexor digitorum profundus (FDP).
 Patients with isolated small finger extensor tendon (EDM) rupture may still be able to extend the small fingers through the EDC or through the juncturae connecting it to the ring finger (Fig. 31-1). However, these patients will not be able to perform independent extension of the small finger with the other fingers flexed.
Patients with isolated small finger extensor tendon (EDM) rupture may still be able to extend the small fingers through the EDC or through the juncturae connecting it to the ring finger (Fig. 31-1). However, these patients will not be able to perform independent extension of the small finger with the other fingers flexed.
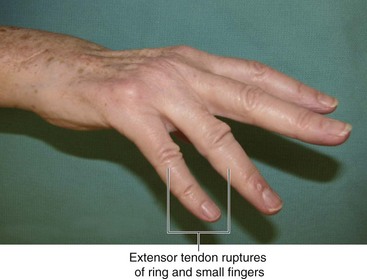
 Patients with rupture of the EDC to one finger may still be able to extend the finger owing to the juncturae connecting it to intact adjoining fingers. However, patients are usually unable to extend the finger when they have ruptured more than one EDC (Fig. 31-2). The inability to extend the finger in RA may also be caused by ulnar subluxation of the extensor tendons over the head of the metacarpal (Fig. 31-3) and rarely is due to posterior interosseous nerve palsy resulting from elbow synovitis. To differentiate between these causes, it is useful to passively extend the finger and ask the patient to hold it there. Patients with tendon rupture or nerve palsy will be unable to maintain the finger in extension, whereas patients with subluxation will be able to do so as the tendon relocates over the metacarpophalangeal (MCP) joint with finger extension. Patients with tendon rupture will also lose the tenodesis effect of finger extension with wrist flexion, whereas the tenodesis effect will be preserved in nerve palsy.
Patients with rupture of the EDC to one finger may still be able to extend the finger owing to the juncturae connecting it to intact adjoining fingers. However, patients are usually unable to extend the finger when they have ruptured more than one EDC (Fig. 31-2). The inability to extend the finger in RA may also be caused by ulnar subluxation of the extensor tendons over the head of the metacarpal (Fig. 31-3) and rarely is due to posterior interosseous nerve palsy resulting from elbow synovitis. To differentiate between these causes, it is useful to passively extend the finger and ask the patient to hold it there. Patients with tendon rupture or nerve palsy will be unable to maintain the finger in extension, whereas patients with subluxation will be able to do so as the tendon relocates over the metacarpophalangeal (MCP) joint with finger extension. Patients with tendon rupture will also lose the tenodesis effect of finger extension with wrist flexion, whereas the tenodesis effect will be preserved in nerve palsy.
 The function of the EPL is tested by asking the patient to lay the palm of the hand flat on the table and then asking the patient to lift the thumb away from the table (retropulsion).
The function of the EPL is tested by asking the patient to lay the palm of the hand flat on the table and then asking the patient to lift the thumb away from the table (retropulsion).
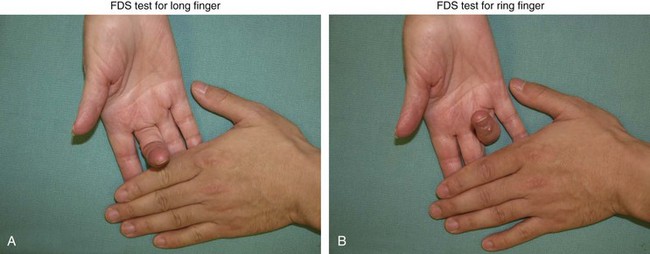
 One must also examine the integrity of the EIP by testing for independent extension of the index finger with the other fingers held in flexion. The function of the FDS and FDP is also checked. The EIP and FDS to the ring and long fingers are often used as motors for tendon transfers in patients with rupture of multiple extensor tendons. Figure 31-4 shows testing for FDS function of the long and ring fingers.
One must also examine the integrity of the EIP by testing for independent extension of the index finger with the other fingers held in flexion. The function of the FDS and FDP is also checked. The EIP and FDS to the ring and long fingers are often used as motors for tendon transfers in patients with rupture of multiple extensor tendons. Figure 31-4 shows testing for FDS function of the long and ring fingers.
Imaging
 It is important to obtain radiographs of the wrist to evaluate the distal radioulnar (DRU), midcarpal, and radiocarpal joints. Pathology involving these joints will also need to be addressed at the time of tendon reconstruction to prevent progressive deformity and rerupture of the reconstructed tendons.
It is important to obtain radiographs of the wrist to evaluate the distal radioulnar (DRU), midcarpal, and radiocarpal joints. Pathology involving these joints will also need to be addressed at the time of tendon reconstruction to prevent progressive deformity and rerupture of the reconstructed tendons.
Surgical Anatomy
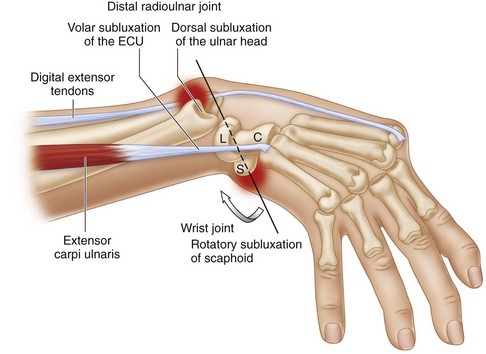
 Tendon rupture in RA occurs as a result of either synovitis or attrition over an eroded bone. The tendon may be directly invaded by the synovial pannus. This occurs in regions where the tendon is covered by tenosynovium (extensor retinaculum, carpal tunnel, and digital flexor sheath). Rupture may also result from ischemia caused by pressure from underlying proliferative synovitis. This occurs in regions where the tendon is in close relation to joints (DRU, radiocarpal, proximal interphalangeal [PIP] joints). Attritional rupture frequently involves the EDM at the ulnar head (Fig. 31-5), EPL at the Lister tubercle, and FPL in the carpal tunnel caused by a flexed scaphoid (see Fig. 31-5). Synovitis between the scaphoid and lunate leads to rupture of the scapholunate ligament and collapse of the scaphoid (scaphoid becomes horizontal with the distal pole protruding into the carpal tunnel).
Tendon rupture in RA occurs as a result of either synovitis or attrition over an eroded bone. The tendon may be directly invaded by the synovial pannus. This occurs in regions where the tendon is covered by tenosynovium (extensor retinaculum, carpal tunnel, and digital flexor sheath). Rupture may also result from ischemia caused by pressure from underlying proliferative synovitis. This occurs in regions where the tendon is in close relation to joints (DRU, radiocarpal, proximal interphalangeal [PIP] joints). Attritional rupture frequently involves the EDM at the ulnar head (Fig. 31-5), EPL at the Lister tubercle, and FPL in the carpal tunnel caused by a flexed scaphoid (see Fig. 31-5). Synovitis between the scaphoid and lunate leads to rupture of the scapholunate ligament and collapse of the scaphoid (scaphoid becomes horizontal with the distal pole protruding into the carpal tunnel).
Treatment Considerations
 Direct repair of ruptured tendons is usually not possible because the ruptured ends are of very poor quality. Additionally, these patients frequently present late, and a tendon graft is also not a reliable option owing to proximal myostatic contraction. A tendon transfer is the preferred option for reconstruction. Depending on the number of ruptured tendons, this may involve a simple end-to-side repair to an intact adjacent tendon or may require transfer of a new motor from the extensor or flexor side (Table 31-1; Fig. 31-6).
Direct repair of ruptured tendons is usually not possible because the ruptured ends are of very poor quality. Additionally, these patients frequently present late, and a tendon graft is also not a reliable option owing to proximal myostatic contraction. A tendon transfer is the preferred option for reconstruction. Depending on the number of ruptured tendons, this may involve a simple end-to-side repair to an intact adjacent tendon or may require transfer of a new motor from the extensor or flexor side (Table 31-1; Fig. 31-6).
 It is important to address the cause of the tendon rupture at the time of tendon reconstruction. This may require tendon and joint synovectomy and procedures to address any joint instability and bony erosions. For example, if the patient has small-finger extensor tendon rupture, it is highly likely that the ring finger extensor tendon will rupture subsequently, and this process will progress, resulting in ruptures of all the extensor tendons to the fingers. Therefore, when a patient has an extensor tendon rupture of the small finger, tendon reconstruction and either tenosynovectomy or distal ulna excision, or a combination of both, must be performed to prevent progressive ruptures of the other tendons.
It is important to address the cause of the tendon rupture at the time of tendon reconstruction. This may require tendon and joint synovectomy and procedures to address any joint instability and bony erosions. For example, if the patient has small-finger extensor tendon rupture, it is highly likely that the ring finger extensor tendon will rupture subsequently, and this process will progress, resulting in ruptures of all the extensor tendons to the fingers. Therefore, when a patient has an extensor tendon rupture of the small finger, tendon reconstruction and either tenosynovectomy or distal ulna excision, or a combination of both, must be performed to prevent progressive ruptures of the other tendons.