Procedure 30 Synovectomy
Indications
Examination/Imaging
Clinical Examination
 Dorsal wrist: Extensor tendon synovitis can clearly be seen and palpated as a soft swelling on the dorsum of the wrist. Isolated dorsal tenosynovitis is painless. When patients with dorsal tenosynovitis complain of pain, one must look for involvement of the radiocarpal or radioulnar joints. Wrist mobility may be limited in this situation. It is also important to assess for the presence of ruptured extensor tendon and differentiate it from subluxation of the extensor tendons over the dorsum of the metacarpophalangeal (MCP) joints.
Dorsal wrist: Extensor tendon synovitis can clearly be seen and palpated as a soft swelling on the dorsum of the wrist. Isolated dorsal tenosynovitis is painless. When patients with dorsal tenosynovitis complain of pain, one must look for involvement of the radiocarpal or radioulnar joints. Wrist mobility may be limited in this situation. It is also important to assess for the presence of ruptured extensor tendon and differentiate it from subluxation of the extensor tendons over the dorsum of the metacarpophalangeal (MCP) joints.
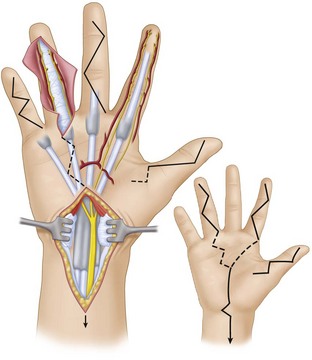
 Palmar aspect of hand: The presence of synovitis over the palmar aspect of the hand is indicated by the presence of (1) swelling (Fig. 30-1), (2) discrepancy between active and passive range of motion (Fig. 30-2), and (3) palpable crepitus along the course of the flexor tendon on active and passive flexion of the digit. This crepitus is best felt by asking the patient to flex the interphalangeal (IP) joints while applying some pressure over the tendon proximal to the A1 pulley of the flexor tendon sheath. The patient may also have triggering of the fingers. Flexor tendon ruptures occur infrequently compared with extensor tendon ruptures. One must also look for carpal tunnel syndrome as a result of proliferative synovitis within the carpal tunnel.
Palmar aspect of hand: The presence of synovitis over the palmar aspect of the hand is indicated by the presence of (1) swelling (Fig. 30-1), (2) discrepancy between active and passive range of motion (Fig. 30-2), and (3) palpable crepitus along the course of the flexor tendon on active and passive flexion of the digit. This crepitus is best felt by asking the patient to flex the interphalangeal (IP) joints while applying some pressure over the tendon proximal to the A1 pulley of the flexor tendon sheath. The patient may also have triggering of the fingers. Flexor tendon ruptures occur infrequently compared with extensor tendon ruptures. One must also look for carpal tunnel syndrome as a result of proliferative synovitis within the carpal tunnel.
Surgical Anatomy
 Synovitis is the hallmark of rheumatoid arthritis (RA), and, in the hand, it involves the synovial lining of the tendon sheath (tenosynovium) and the joint. Flexor tendons are covered by the tenosynovium under the carpal tunnel and in the digital flexor sheath, whereas extensor tendons are covered by tenosynovium only under the extensor retinaculum. Synovitis of the hand involves the extensor tendons more frequently than the flexor tendons.
Synovitis is the hallmark of rheumatoid arthritis (RA), and, in the hand, it involves the synovial lining of the tendon sheath (tenosynovium) and the joint. Flexor tendons are covered by the tenosynovium under the carpal tunnel and in the digital flexor sheath, whereas extensor tendons are covered by tenosynovium only under the extensor retinaculum. Synovitis of the hand involves the extensor tendons more frequently than the flexor tendons.
 Extensor tendon involvement is frequently seen over the dorsum of the wrist and results from synovitis progressing from the distal radioulnar joint and tenosynovitis under the extensor retinaculum. In contrast, the changes in the extensor tendon seen at the interphalangeal joints are caused by the underlying joint synovitis and not tenosynovitis.
Extensor tendon involvement is frequently seen over the dorsum of the wrist and results from synovitis progressing from the distal radioulnar joint and tenosynovitis under the extensor retinaculum. In contrast, the changes in the extensor tendon seen at the interphalangeal joints are caused by the underlying joint synovitis and not tenosynovitis.
 Three main groups of flexor tenosynovitis can be distinguished: isolated carpal tenosynovitis (20%), palmodigital tenosynovitis (50%), and diffuse tenosynovitis (30%). The index, long, and small fingers are most frequently involved. A flexor tendon rupture in the digital flexor sheath is almost always secondary to infiltrative synovitis and usually involves the flexor digitorum superficialis (FDS) at the proximal interphalangeal (PIP) joint. This is probably because the FDS splits into two slips in the distal third of the proximal phalanx. This decreases the thickness of the tendon and increases the surface area in contact with the invading synovium.
Three main groups of flexor tenosynovitis can be distinguished: isolated carpal tenosynovitis (20%), palmodigital tenosynovitis (50%), and diffuse tenosynovitis (30%). The index, long, and small fingers are most frequently involved. A flexor tendon rupture in the digital flexor sheath is almost always secondary to infiltrative synovitis and usually involves the flexor digitorum superficialis (FDS) at the proximal interphalangeal (PIP) joint. This is probably because the FDS splits into two slips in the distal third of the proximal phalanx. This decreases the thickness of the tendon and increases the surface area in contact with the invading synovium.
Tenosynovectomy
1 Digital Flexor Synovectomy
Exposures
 A Bruner type incision is made in the fingers extending onto the distal palm (Fig. 30-3).
A Bruner type incision is made in the fingers extending onto the distal palm (Fig. 30-3).
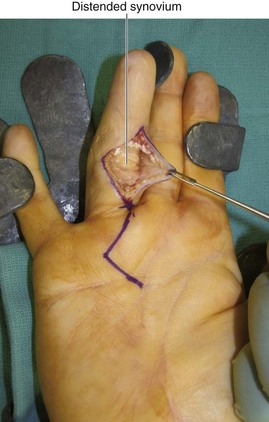
 The skin flaps are raised in a plane superficial to the flexor tendon sheath. This brings into view the sausage-shaped mass of distended synovium (Fig. 30-4).
The skin flaps are raised in a plane superficial to the flexor tendon sheath. This brings into view the sausage-shaped mass of distended synovium (Fig. 30-4).
Procedure
Step 1: Synovectomy
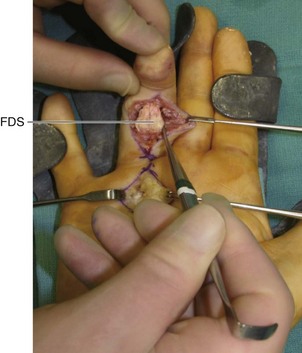
 Flexor tendon synovectomy is performed by pulling the FDS and flexor digitorum profundus (FDP) tendons alternatively through the openings in the tendon sheath. The area of tenosynovitis can then be excised from each tendon using a combination of sharp and blunt dissections (Fig. 30-5).
Flexor tendon synovectomy is performed by pulling the FDS and flexor digitorum profundus (FDP) tendons alternatively through the openings in the tendon sheath. The area of tenosynovitis can then be excised from each tendon using a combination of sharp and blunt dissections (Fig. 30-5).
Step 1 Pitfalls
The slips of the FDS may be infiltrated with tenosynovitis, and the surgeon may be tempted to excise the FDS tendon, which should be avoided because of the progressive nature of the disease. The FDS is the prime flexor of the PIP joint, and excising it may result in a swan neck deformity.
Care is taken not to injure the neurovascular bundles and resect the tendon pulleys accidentally.
Step 2: Checking Passive Range of Motion
 After the tenosynovectomy, the smooth gliding of tendons (FDS and FDP) is confirmed by flexion and extension of the fingers (Fig. 30-6).
After the tenosynovectomy, the smooth gliding of tendons (FDS and FDP) is confirmed by flexion and extension of the fingers (Fig. 30-6).
Step 2 Pearls
If surgery is performed with the patient under local anesthesia or a Bier block, active range of motion can be visualized and any residual diseased areas addressed.
If “catching” is found when testing for tendon excursion after tenosynovectomy, check for flexor tendon nodules in digits and/or palm.
If triggering of finger persists after tenosynovectomy, an A1 pulley release is performed.
Step 2 Pitfalls
The release of the A1 pulley may contribute to the MCP joint ulnar drift deformity, especially for the index and long fingers, because of the oblique line of pull of the long flexors for these digits. Some investigators recommend resection of one slip of the FDS to provide greater space for passage of the FDP instead of A1 pulley release.