Chapter 3 Patient Education, Decisions, and Informed Consent
Decisions affect patient outcomes and the patient experience more than any surgical technique or implant device. A staged, repetitive system of patient education, integrated with detailed informed consent documents, best assures optimal patient education and informed consent.1 Optimal decisions require knowledge applied through valid decision making processes. Few, if any, prospective breast augmentation patients begin the patient experience knowing what they need to know to make optimal decisions for an optimal outcome. Even fewer patients understand alternative decision processes and decision pathways that lead to predictably optimal outcomes in breast augmentation. Current reoperation rates in United States Food and Drug Administration (FDA) and Health Canada studies,2–4 and the reasons for reoperations and suboptimal outcomes support the previous statements. Data in FDA premarket approval (PMA) studies and current rates of litigation suggest a need and opportunities for surgeons to provide patients better and more information and to improve patient education, decision making, and informed consent prior to breast augmentation.
Valid Patient Educational Processes
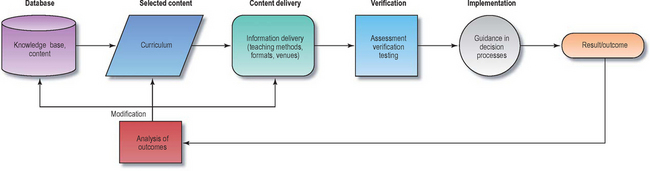
Optimal outcomes require optimal processes. The processes of patient education and informed consent should logically follow established models of proved educational models and processes that meet legal requirements for informed consent.Figure 3-1 illustrates components that are essential to any valid educational model or process.
Processes of patient education and informed consent must be comprehensive and carefully documented to assure optimal medicolegal compliance. These requirements can be accomplished while optimizing surgeon time use by implementing a system of information documents, patient choice documents, and informed consent documents that are integrated and used at sequential patient encounters. The system currently in use in the author’s practice has evolved over a 26 year period, has been subjected to detailed legal scrutiny, and has been peer reviewed and published in the journal Plastic and Reconstructive Surgery.1
The primary source of content for our comprehensive patient education is our book entitled The Best Breast, first published in 1999, and now in its second edition. This book is the most comprehensive source of information about breast augmentation for patients, and the second edition is extensively referenced to provide scientific validity for the content based on our peer reviewed and published articles in Plastic and Reconstructive Surgery. The book is available at bookstores and through http://www.Amazon.com, or by calling our office at (+1)214-220-2712. The book website, http://www.thebestbreast.com, contains extensive content excerpts from the book and additional references and links for patients seeking information about breast augmentation.
To best understand how this comprehensive system actually applies in clinical practice, surgeons should first read the original article from the journal or online at the journal’s website, http://www.plasreconsurg.com. With the overview the article provides, the surgeon should then read in detail each of the individual documents that apply at each patient encounter in order, as a patient would read them. Each of these documents is available in Adobe Acrobat™ pdf format in the Resources folder on the DVDs that accompany this book. Surgeons can use these resources for review or as templates to individualize similar documents.
Table 3-1 lists each of the documents in the author’s patient education in the order in which the documents are used at each patient encounter. Thoroughly understanding this system requires that surgeons read this chapter, and then read each of the informed consent documents in sequence, paying special attention to when and how the documents apply at each patient encounter. A summary of the patient education process will provide a basis for understanding how this document system can be comprehensive, staged, and repetitive, while maximizing surgeon efficiency.
Table 3-1 An overview of the informed consent process and documents
| Patient encounter | Personnel | Document name and number |
|---|---|---|
| 1. Initial patient call | Patient coordinator and/or patient educator | Surgeon’s written information of choice, in the author’s practice, the book entitled The Best Breast |
| 2. Patient educator consult | Patient educator | |
| 3. Surgeon consultation | Surgeon | |
| 4. Documents packet provided to patient when surgery scheduled | Surgery scheduling coordinator | 14. Informed Consent for Patients Desiring Augmentation Mammaplasty and Who Have a Family History of Breast Cancer 16. Informed Consent for Patients Desiring Augmentation with a Larger Implant than Dr. [Surgeon’s Name] Feels is Optimal for the Patient’s Tissues 17. Informed Consent for Patients Desiring Augmentation Mammaplasty Through a Belly Button (Umbilical) Incision |
* Specialized informed consent documents. One or more may be used depending on patient’s specific choices, medical history, or tissue requirements. Each document listed in the right column is available in the Re sources folder or the DVDs accompanying the book.
Applying Education and Informed Consent Systems in Practice Management
Patient Encounters During a Staged, Repetitive Education and Informed Consent Process
In our practice, four patient encounters occur during the patient education and informed consent process (Table 3-1):
Initial Telephone Call and Information Provided to the Patient
Following the initial patient phone call to the office, the author provides each patient with a copy of his book entitled The Best Breast (available online, at most bookstores, or by contacting the author’s office) and requires that the patient acknowledge having read the book prior to a patient educator consultation that precedes the surgeon consultation. If a patient is unwilling to attempt to read the materials provided, we usually suggest that the patient seek treatment elsewhere. If the patient makes an effort to read and digest the information, we are always willing to provide additional information and support to complement the initial information. While generic materials traditionally provided to patients by professional societies and other sources are helpful, none provides the depth of information that a surgeon can provide by committing time and resources to provide much more detailed information backed by peer reviewed and referenced data. More importantly, no generic materials to our knowledge provide meaningful decision support algorithms or processes, and none provides any significant level of testing or verification to assure a specific level of patient understanding and acceptance of responsibility for patient requests and choices.
Patient Educator Consultation
The patient educator DVD content provides a framework for patient decision making that encourages the patient to choose from realistic alternatives that seek to minimize “gray areas” and present more “black and white” alternatives. The DVD also encourages the patient to list questions or topics for further discussion with the patient educator. While viewing the DVD in stages, the patient reads and signs, paragraph by paragraph, the detailed informed consent document entitled “My Preferences and Information I Fully Understand and Accept” that sequentially asks the patient to make choices after reading the book and hearing verbal presentations on the DVD. These choices and preferences are not final, but provide documentation that the patient has received and understands essential printed and visual information, and further documents the patient’s decision processes. The Choices and Preferences document asks several key questions in two or three different ways, allowing the staff and surgeon to judge the consistency of a patient’s answers and the knowledge level of the patient. Equally importantly, the answers in the document enable staff and surgeon to identify inconsistencies or hidden patient agendas that may or may not be realistic in the patient’s individual clinical setting.
The Surgeon Consultation
Prior to the surgeon consultation, the patient has read an extensive amount of information, reviewed information in stages, viewed a patient education DVD, stated her preliminary preferences and choices on the Choices and Preferences document, and completed a patient educator consultation to review and clarify the information and answer questions. With this preparation, the surgeon consultation can focus on quantifying the patient’s tissue characteristics and breast measurements, and answering the key question, “Knowing the patient’s preferences stated on the Choices and Preferences document, and quantifying patient tissue characteristics, can the surgeon predictably deliver what the patient is requesting with optimal safety and efficacy long-term?” The patient education, decision making, and informed consent process helps the patient reconcile her wishes with the realities of her tissues. If any of her requests are suboptimal given her individual tissue characteristics, surgeon and patient reconcile potential compromises, and finalize choices during the surgeon consultation.
During the surgeon consultation, the surgeon completes five basic measurements and makes five critical decisions in less than 5 minutes using the High Five™ System. This system is discussed in detail inChapter 4. Using this quantifiable, efficient system, the surgeon completes choices of pocket location (soft tissue coverage), implant volume, implant type, position of the inframammary fold to set intraoperatively, and incision location. The surgeon can ask the patient to initial these choices at the time of the surgeon consultation, assuring another level of documentation of the patient’s choices.
The funnel analogy—understanding what is optimal fill for each individual patient
The wider your breast, and the greater your skin stretch, the greater the amount of fill that we must place into your breast to fill it adequately for an optimal result. If we stop short of the optimal amount of fill, your upper breast will not be adequately filled, and your breast may have a “rock in a sock” appearance. In the opposite situation, if you have a narrow breast and minimal skin stretch, your breast does not require and will not accommodate as much fill. If we attempt to place excessive fill in your breast, you may have excessive upper breast fullness and bulging with a breast that appears more like a basketball compared to a natural breast.
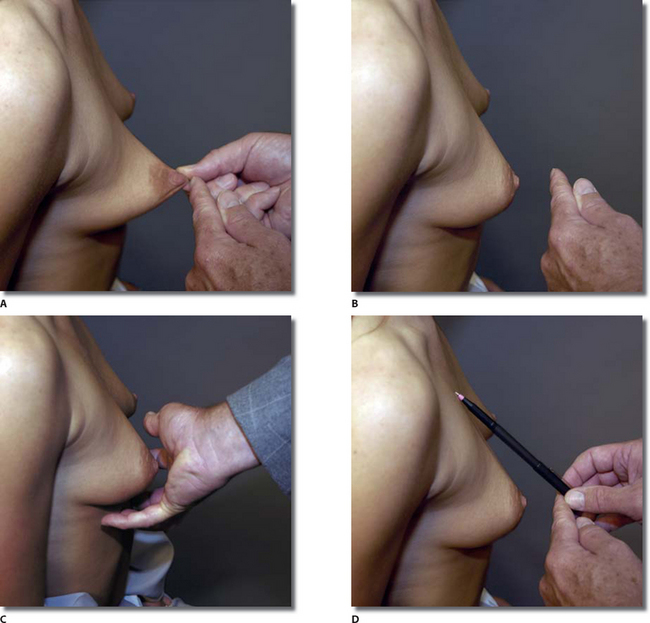
Imagine that we have a funnel in the top of your breast. As we pour fill into the funnel, the lower portion of your breast fills first until it reaches its limit of stretch. This may be a bit uncomfortable, but let’s determine the maximum amount your skin will stretch forward by grasping the skin and pulling it until you feel discomfort and the skin stops (Figure 3-2, A, B). [During this maneuver, the surgeon grasps the areolar skin immediately beside the nipple and stretches it maximally forward, noting the location of maximal stretch with a fingernail (Figure 3-2, B), and then releases the skin. At this maximum stretch distance from the breast, the surgeon cups the hand around the lower pole of the breast at a distance approximately equal to the maximal skin stretch (Figure 3-2, C), and continues the dialog.]
If I cup my hand at an equal distance around your lower breast at this point of maximal stretch, if you will look down, you can visually get an idea of how full your lower breast will be at maximal skin stretch without overstretching or damaging the skin (Figure 3-2, C). From this point of maximal stretch, I will align my pen onto your upper chest (Figure 3-2, D), and you can get an idea of the area under the pen that will be filled in the upper breast.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree