Procedure 20 Tendon Transfers for Radial Nerve Palsy
![]() See Video 16: Standard Tendon Transfer Sequence for Radial Nerve Palsy
See Video 16: Standard Tendon Transfer Sequence for Radial Nerve Palsy
See Video 17: Alternate Tendon Transfer Sequence for Radial Nerve Palsy When PL Is Absent
Examination/Imaging
Clinical Examination
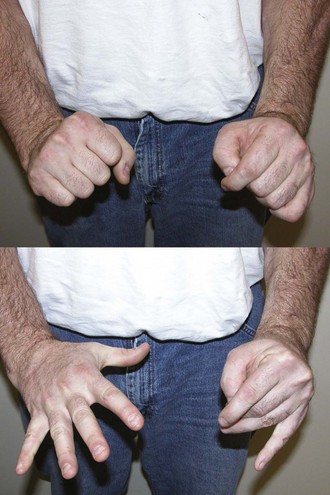
 Functional deficit: The loss of function in radial nerve palsy results from the wrist drop deformity, which causes an inability to extend the wrist and the finger metacarpophalangeal (MCP) joints and to extend and abduct the thumb (Fig. 20-1). The loss of wrist extension weakens power grip, and the loss of finger and thumb extension makes it difficult to grasp objects. It is important to differentiate radial nerve palsy (above the elbow) from posterior interosseous nerve (PIN) palsy (below the elbow). The extensor carpi radialis longus (ECRL) receives its innervation by a branch of the radial nerve that arises above the elbow. It is therefore spared in a lesion of the PIN, and patients can extend the wrist, although with radial deviation (Fig. 20-2).
Functional deficit: The loss of function in radial nerve palsy results from the wrist drop deformity, which causes an inability to extend the wrist and the finger metacarpophalangeal (MCP) joints and to extend and abduct the thumb (Fig. 20-1). The loss of wrist extension weakens power grip, and the loss of finger and thumb extension makes it difficult to grasp objects. It is important to differentiate radial nerve palsy (above the elbow) from posterior interosseous nerve (PIN) palsy (below the elbow). The extensor carpi radialis longus (ECRL) receives its innervation by a branch of the radial nerve that arises above the elbow. It is therefore spared in a lesion of the PIN, and patients can extend the wrist, although with radial deviation (Fig. 20-2).
 Sensation: Sensory loss in the areas innervated by the superficial radial nerve (anatomic snuffbox and dorsum of first web) can help differentiate a radial nerve lesion from a lesion of the PIN, which should have preserved sensation over the dorsum of the first web (Fig. 20-3).
Sensation: Sensory loss in the areas innervated by the superficial radial nerve (anatomic snuffbox and dorsum of first web) can help differentiate a radial nerve lesion from a lesion of the PIN, which should have preserved sensation over the dorsum of the first web (Fig. 20-3).
 Joints: To get a good result from the tendon transfer, patients must have good passive range of motion at the wrist and the MCP joint. One of the common transfers uses wrist flexors for obtaining finger and thumb MCP joint extension. The excursion of wrist flexors is approximately 33 mm, whereas finger extension requires a tendon excursion of 50 mm. This difference in excursion is obtained by the natural tenodesis effect, and patients are able to obtain full finger extension when the wrist is flexed.
Joints: To get a good result from the tendon transfer, patients must have good passive range of motion at the wrist and the MCP joint. One of the common transfers uses wrist flexors for obtaining finger and thumb MCP joint extension. The excursion of wrist flexors is approximately 33 mm, whereas finger extension requires a tendon excursion of 50 mm. This difference in excursion is obtained by the natural tenodesis effect, and patients are able to obtain full finger extension when the wrist is flexed.
 Selection of motor: Our preferred motors are as follows. Patients with PIN palsy do not require a transfer for wrist extension because the ECRL is functional.
Selection of motor: Our preferred motors are as follows. Patients with PIN palsy do not require a transfer for wrist extension because the ECRL is functional.
Imaging
 Electrodiagnostic studies are often used to confirm the diagnosis of a nerve problem. For radial nerve palsy, these nerve studies are not particularly useful because muscle testing and careful examination should be able to identify the functional deficits and the available tendons that can be transferred.
Electrodiagnostic studies are often used to confirm the diagnosis of a nerve problem. For radial nerve palsy, these nerve studies are not particularly useful because muscle testing and careful examination should be able to identify the functional deficits and the available tendons that can be transferred.
Surgical Anatomy
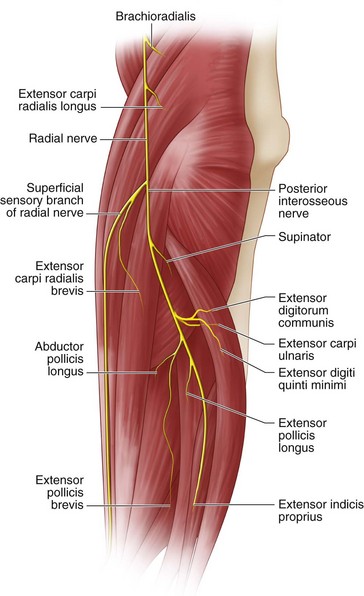
 The radial nerve divides into the superficial radial nerve and the posterior interosseous nerve at the level of the lateral epicondyle (about 1 to 2 cm above the elbow joint). It gives off branches that innervate the brachioradialis (BR) and the ECRL before this division. The ECRB has variable innervation that can arise from the radial nerve, superficial radial nerve, or PIN. The remaining extensor compartment muscles are innervated in the following order by the PIN: supinator, EDC, extensor carpi ulnaris (ECU), extensor digiti quinti minimi (EDQM), abductor pollicis longus (APL), extensor pollicis longus (EPL), extensor pollicis brevis (EPB), and extensor EIP (Fig. 20-4).
The radial nerve divides into the superficial radial nerve and the posterior interosseous nerve at the level of the lateral epicondyle (about 1 to 2 cm above the elbow joint). It gives off branches that innervate the brachioradialis (BR) and the ECRL before this division. The ECRB has variable innervation that can arise from the radial nerve, superficial radial nerve, or PIN. The remaining extensor compartment muscles are innervated in the following order by the PIN: supinator, EDC, extensor carpi ulnaris (ECU), extensor digiti quinti minimi (EDQM), abductor pollicis longus (APL), extensor pollicis longus (EPL), extensor pollicis brevis (EPB), and extensor EIP (Fig. 20-4).
Exposures
 A 6-cm longitudinal incision is made over the volar radial aspect of the mid-forearm (Fig. 20-5). This incision is centered over the palpable musculotendinous junction of the ECRB and ECRL. The forearm fascia is divided, and the tendons of ECRB and ECRL are identified. The BR is identified radial to the ECRL and retracted ulnarly along with the ECRL. The superficial branch of the radial nerve should be identified under the BR and protected. This will bring into view the insertion of the PT (Fig. 20-6).
A 6-cm longitudinal incision is made over the volar radial aspect of the mid-forearm (Fig. 20-5). This incision is centered over the palpable musculotendinous junction of the ECRB and ECRL. The forearm fascia is divided, and the tendons of ECRB and ECRL are identified. The BR is identified radial to the ECRL and retracted ulnarly along with the ECRL. The superficial branch of the radial nerve should be identified under the BR and protected. This will bring into view the insertion of the PT (Fig. 20-6).
 A 4-cm longitudinal incision is made over the Lister tubercle (see Fig. 20-5). The extensor retinaculum is exposed and the third compartment opened to free the EPL. The EIP, EDC, and EDQM tendons are identified proximal to the extensor retinaculum.
A 4-cm longitudinal incision is made over the Lister tubercle (see Fig. 20-5). The extensor retinaculum is exposed and the third compartment opened to free the EPL. The EIP, EDC, and EDQM tendons are identified proximal to the extensor retinaculum.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree