Cutaneous Manifestations of Myelogenous Leukemia
Myelogenous leukemias are a spectrum of diseases encompassing chronic myeloproliferative diseases, myelodysplastic disorders, and acute myeloid leukemias and related disorders. The classification of these neoplasms has been considerably changed in recent time, and the World Health Organization (WHO) Classification of Tumours of Haematopoietic and Lymphoid Tissues takes into consideration genetic features along with conventional clinical, histopathologic, and phenotypic aspects [1]. However, most reports on skin involvement pre-date the new classification, so the frequency of cutaneous involvement in the different subtypes is not known. Skin manifestations are more common in patients with more mature forms of myeloid leukemia, but can be observed in all subtypes of it, as well as in a small percentage of patients with chronic myelogenous leukemia and rarely in those with myelodysplastic syndromes [2–14]. Specific skin involvement has also been observed in the context of therapy-related myeloid leukemia [15].
In general, in patients with chronic myelogenous leukemia or myelodysplastic syndromes skin involvement is related to transformation or progression of the chronic myeloid or myelodysplastic disorder. In this context, it is interesting to note that overlapping myeloid and lymphoid features may be observed in chronic myelogenous leukemia, in which blast crisis in 10% of the cases reveals a B- or, more rarely, a T-cell phenotype (“transdifferentiation” – see also Chapter 1).
Cases showing isolated extramedullary tumors with myeloid differentiation have been denominated chloroma or granulocytic sarcoma in the past, and are currently referred to as myeloid sarcomas [16–19]. Myeloid sarcoma may precede or be concomitant with myelogenous leukemia.
In the last few years, some publications dealing with blastic plasmacytoid dendritic cell neoplasms showed that in some patients a relationship between this entity and myelogenous leukemia exists (see Chapter 21). Indeed, in the WHO classification blastic plasmacytoid dendritic cell neoplasm is mentioned in the chapter on acute myeloid leukemia and related precursor neoplasms [1].
Clinical Features
The majority of patients are adults who present with multiple, localized, or generalized papules, plaques, and nodules with a characteristic reddish-brown or violaceous color in the context of a known leukemia (Fig. 20.1). Involvement of the mucosal regions is common (Fig. 20.2). Cases have been reported in children and even neonates (Fig. 20.3) [20, 21]. Interestingly, a neonate with typical “blueberry muffin” clinical presentation and skin infiltrates of myelomonocytic leukemia did not have any extracutaneous manifestation at staging, suggesting that “aleukemic” leukemia cutis may be observed in newborns, too [22]. Spontaneous regression of skin lesions without treatment has been observed in congenital myelogenous leukemia, but is a rare event [23].
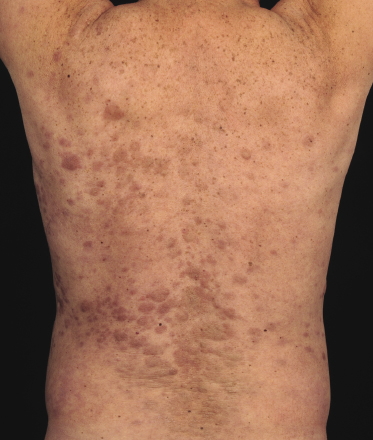


Diagnosis of specific cutaneous infiltrates may be difficult in cases presenting with unusual clinical features such as solitary skin nodules, maculo-papular eruptions clinically resembling drug or viral eruptions, vasculitis, or other uncommon presentations (Fig. 20.4) [2]. In this context, it should be noted that in some patients “inflammatory dermatoses-like” cutaneous eruptions have been observed as the first sign of relapse of treated myelogenous leukemia, underlining the need for precise clinicopathologic correlation and for a high grade of suspicion in these patients [24].
As for other types of leukemia, specific manifestations have been observed at the site of cutaneous inflammation [25−29]. This phenomenon seems to be more frequent for lesions of Sweet’s syndrome, but has been observed also at sites of psoriasis, basal cell carcinoma, needle puncture, and infusion of gabexate mesilate that had leaked from the vein [25–29].
In a distinct proportion of patients specific skin infiltrates represent the first clinical manifestation of the disease, preceding blood and/or bone marrow involvement by weeks or even months (“aleukemic” leukemia cutis) [2, 30, 31]. These patients should be managed in the same way as those with cutaneous manifestations of known myelogenous leukemia.
Histopathology, Immunophenotype, and Molecular Genetics
Histopathology
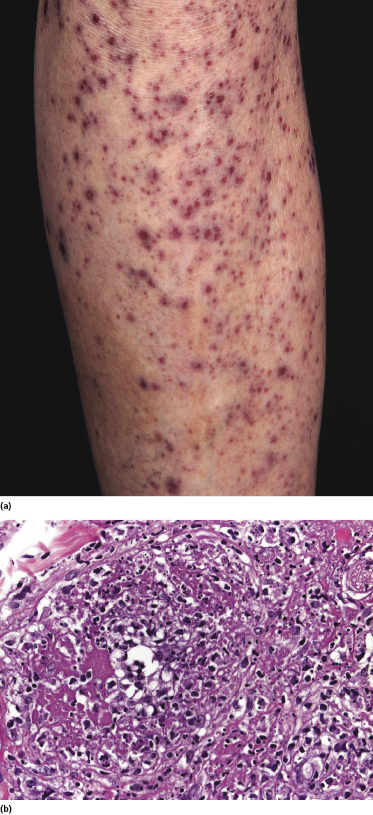
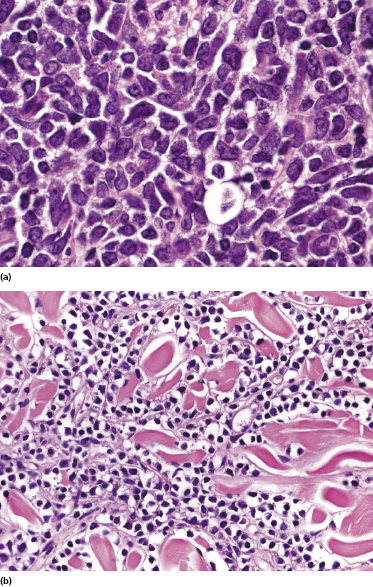
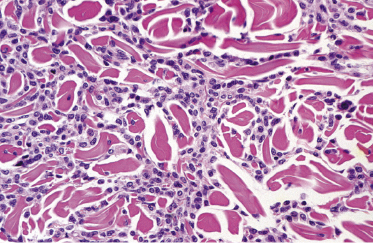
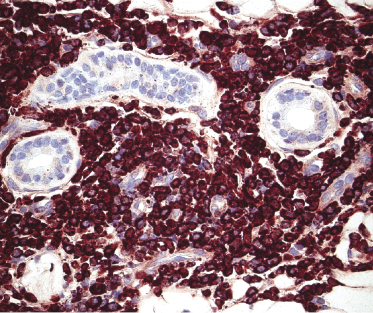
In most instances there are no major differences in the histopathologic features of specific skin involvement by acute or chronic myelogenous leukemia [2]. Cutaneous lesions show mild, moderate, or dense, diffuse or nodular dermal infiltrates, often with perivascular and periadnexal accentuation and sparing of the upper papillary dermis. Involvement of the subcutis is common. In most cases the infiltrate is composed of medium-sized, round to oval cells with a slightly eosinophilic cytoplasm and distinct, sometimes indented, bilobular or kidney-shaped basophilic nuclei (atypical monocytoid cells) (Fig. 20.5a). Large cells may also be seen. In more differentiated subtypes of acute myeloid leukemia the nuclei are smaller and the cytoplasm is less prominent, and the cells may resemble pleomorphic lymphocytes (Fig. 20.5b). Variable numbers of mitotic figures (including atypical mitoses) and apoptotic cells can be found. Reactive cells (e.g., lymphocytes, mast cells) are present in some cases. A granulomatous reaction may also be observed (Fig. 20.6) [2, 32, 33].
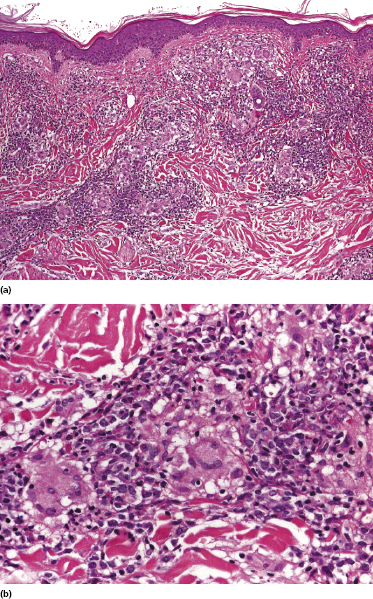
Prominent single files of neoplastic cells between collagen bundles can be observed in the majority of cases (“Indian filing”) (Fig. 20.7). A distinctive “figurate” pattern characterized by concentric layering of neoplastic cells around blood vessels and adnexal structures is frequently found (Fig. 20.8).
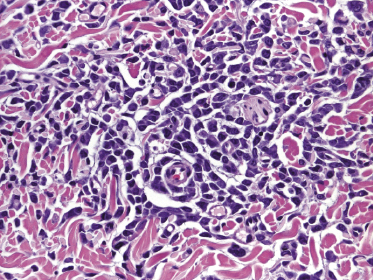
In rare cases, an angiocentric (“vasculitic”) pattern with destruction of the vessels may be observed, mimicking the picture of cutaneous vasculitis or of other angiocentric/angiodestructive lymphomas (Fig. 20.4b). In some of these cases the clinical presentation, too, is reminiscent of leucocytoclastic vasculitis (“palpable purpura”) (Fig. 20.4a). Phenotypic features are identical to those observed in conventional lesions of the disease, thus allowing a proper classification of these cases.
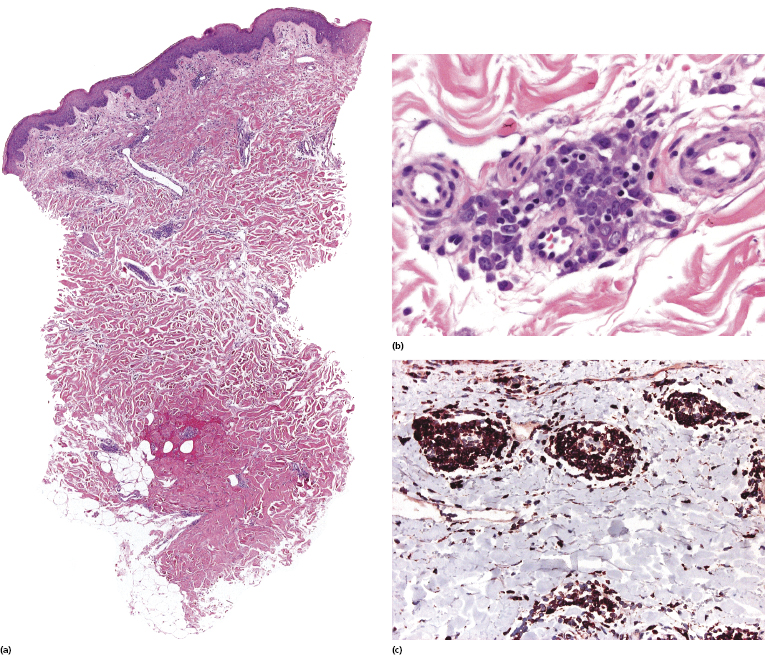
Early cutaneous manifestations of myeloid leukemia may mimic an inflammatory dermatosis both clinically and histopathologically, and may be very difficult to diagnose (Fig. 20.9) [24]. Although the infiltrate may be very sparse, cytomorphological and phenotypic features allow one to make the correct diagnosis. Skin lesions with minimal infiltrates may be observed also as the first sign of relapse of myeloid leukemia in complete remission.
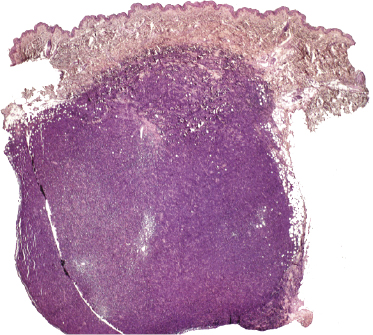
Cutaneous lesions of myeloid sarcoma present with large cutaneous–subcutaneous tumors composed of myeloblasts or monoblasts (Fig. 20.10) [19, 34].
Immunophenotype
The phenotype of cutaneous lesions depends on the type of myelogenous leukemia. Markers that are usually expressed by neoplastic cells include lysozyme, myeloperoxidase, CD13, CD14, CD15, CD33, CD43, CD45, and CD68 (Fig. 20.11), but some cases may show positivity for only a few of these antigens. In particular, CD68 and CD43 (this last marker also stains T lymphocytes and must be evaluated in conjunction with other T-cell markers) are positive in most cases of cutaneous myelogenous leukemia. CD163 is expressed in 30–40% of cases. Staining for naphtol-ASD-chloracetate-esterase (NASDCl, Leder stain) is positive mainly in cases with a mature phenotype, but tends to be negative in more immature cells. Staining for CD56 is found in a minority of cases only; however, since positive cases exist, this marker cannot be used for reliable differentiation from lesions of blastic plasmacytoid dendritic cell neoplasm [2, 6, 35]. As skin lesions of myelogenous leukemia are commonly positive for CD4 and rarely for CD123, a distinction between these two entities may be very difficult. In addition, cases of myelogenous leukemia evolving into blastic plasmacytoid dendritic cell neoplasm have been reported (for a detailed discussion of differential diagnostic features see Chapter 21) [36, 37]. Neoplastic cells in some cases may be positive for S100 protein, thus representing a pitfall in the differential diagnosis with histiocytic disorders (e.g., Langerhans cell histiocytosis) if complete phenotypic analyses are not carried out.
There seems to be no clear-cut correlation between features seen in specific skin infiltrates and the subtype of the underlying myelogenous leukemia. In addition, the phenotype may be different in bone marrow and skin lesions of patients with acute myeloid leukemia involving the skin [38].
Molecular Genetics
Interphase fluorescence in situ hybridization (FISH) analysis has been used to confirm trisomy 8 in cutaneous lesions of several patients with myelogenous leukemia. Other studies revealed similar chromosomal aberrations in the bone marrow and the skin, demonstrating the clonal nature of bone marrow and cutaneous infiltrates. The same t(15;17)(q22;q12) rearrangement has been detected in bone marrow and skin lesions of a case of acute promyelocytic leukemia, confirming that FISH may be an adjunctive tool for specific diagnosis of cutaneous infiltrates [39].
Treatment and Prognosis
The skin manifestations are managed by treating the underlying myelogenous leukemia. Patients with “aleukemic leukemia cutis” should be managed in the same way as patients with blood and/or bone marrow involvement, as the disease inevitably progresses over short periods of time (usually less than 1 year, rarely longer) [40].
There seems to be no difference in survival between patients with specific skin manifestations of acute or chronic myelogenous leukemia. The course is aggressive and survival is usually of a few months only.

Full access? Get Clinical Tree


