Chapter 2 Ten Essentials
Ten Essentials to Optimize Patient Outcomes
Proved processes currently enable surgeons to optimize breast augmentation outcomes according to principles of evidence based outcomes analysis.1–11 Using principles of process engineering and quality control, surgeons can evaluate and apply 10 essentials derived from proved processes to redefine patient outcomes long-term. The processes that have produced a redefined level of patient experience and outcome in breast augmentation are detailed in the chapters of this book. Table 2-1 lists 10 essential processes that are required to predictably deliver an optimal patient experience, recovery, and outcome.
Table 2-1 Ten essential processes for optimal patient experience, recovery, and outcome
| 1. | Prioritize evidence based outcomes analysis and surgeon accountability |
| 2. | Prioritize and optimize patient education, informed consent, and patient accountability |
| 3. | Optimize surgeon education and process implementation using proved educational models, modern technology, verifiability, and surgeon incentives |
| 4. | Prioritize and protect patients’ tissues long-term by choosing implant pocket location to assure optimal long-term tissue coverage of the implant and by avoiding implant sizes or projection that are likely to cause excessive stretching, tissue thinning, and parenchymal atrophy |
| 5. | Implement objective, tissue based clinical evaluation, preoperative decisions, operative planning and implant selection |
| 6. | Prioritize and consider implant design, filler distribution dynamics, and implant–soft tissue dynamics during preoperative patient education, implant selection, and operative planning |
| 7. | Design and dissect the implant pocket to “fit” the implant selected |
| 8. | Minimize trauma and bleeding, eliminate blunt dissection, and apply prospective hemostasis principles |
| 9. | Optimize outcomes prospectively by managing factors that speed recovery |
| 10. | Manage untoward occurrences using defined processes; define end points for implant removal without replacement |
The FDA, patients, and patient advocates evaluate optimal outcomes based on objective data from premarket approval (PMA) studies. PMA studies are the most scientifically constructed and stringently monitored studies on breast augmentation. For more than two decades, PMA data established an unenviable track record of 15–20% reoperation rates within 3 years of augmentation.12–14 Fortunately, that track record is improving, and proved processes are available that enable surgeons to deliver a 3% reoperation rate with up to 7 year followup,2,3,5,10 and a zero percent reoperation rate at 3 years in a PMA series of 50 consecutive patients.11
1. Prioritize evidence based outcomes analysis and surgeon and patient accountability
For the past two decades, most breast augmentation outcomes data in peer reviewed and published studies as well as anecdotal reports indicated a high level of patient satisfaction and low reoperation rates. Surgeons introduced and refined operative techniques including axillary and umbilical incision approaches and endoscopic pocket dissection. During these two decades, however, two things did not improve appreciably—patients’ perioperative experience and recovery, and reoperation rates. Incredibly high reoperation rates within just 3 years of augmentation were exposed in data from FDA saline PMA studies.12–14 FDA Advisory Panel members and patient advocate representatives strongly criticized these reoperation rates and suggested a need for more scientifically constructed studies, long-term followup, evidence based outcomes analysis, and patient and surgeon accountability including a data registry for augmentation.
2. Prioritize and optimize patient education, informed consent, and patient accountability
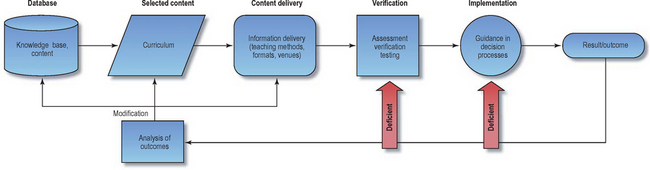
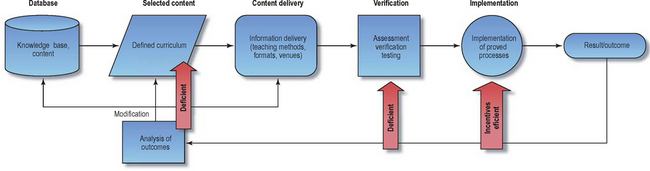
Most current patient education methods and materials provided by professional organizations and surgeons do not optimally address two specific areas that are critically important to optimizing patient education—verifiability or testing to assess whether patients have assimilated critical information, and proved decision support processes to assure decision making pathways that have been shown to optimize outcomes and minimize reoperation rates (Table 2-2). Regardless of the amount of information provided to patients, absent some form of testing or verification to assure their assimilation of the information, the patient never builds an optimal knowledge base. Absent specific guidance in decision processes using processes that have been shown to improve outcomes, patients are unlikely to make optimal choices that ensure optimal long-term outcomes.
Table 2-2 Patient education basic processes and current deficiencies.
Assuming that surgeons optimize all of the previously mentioned factors, patients may nevertheless make requests, choices, or decisions that may adversely affect their long-term outcomes. A common example is requesting an implant size or dimensions that exceed the base width of available soft tissue coverage, or that may excessively stretch or thin envelope tissues or cause parenchymal atrophy in the future. Surgeons cannot predict or control some of these factors. Patients must be accountable for their requests and choices, provided they have been given optimal education and decision support. Processes to assure this accountability are detailed inChapter 4. A third critically deficient area in patient education and informed consent is documenting patient requests and decisions after optimal education. This documentation can be integrated into the educational process in a staged, repetitive manner that provides information, decision support, and line item documentation of patient choices to assure patient and surgeon accountability.7 All of the documents in this system are included in the Resources folder on the DVDs that accompany the book for surgeons to use or modify to suit individual practice preferences.
3. Optimize surgeon education and process implementation using proved educational models, modern technology, verifiability, and surgeon incentives
Meaningful impact to improve outcomes for significant numbers of patients requires a comprehensive approach to surgeon education that integrates essential components of valid education models that have proved successful in industry and medicine. Three critical components are largely absent in current surgeon education and implementation of proved processes: (1) a defined curriculum derived from a knowledge base of reviewed and published processes that have been shown to impact outcomes, (2) verifiability of information exchange by proved testing methodologies (in venues or online), and (3) incentives (positive or negative) to encourage surgeons to implement proved processes (Table 2-3).
Table 2-3 Deficiencies in surgeon education and implementation of proved processes
4. Prioritize and protect patients’ tissues long-term by choosing implant pocket location to assure optimal long-term tissue coverage of the implant and by avoiding implant sizes or projection that are likely to cause excessive stretching, tissue thinning, and parenchymal atrophy
These decision processes are detailed inChapter 9.
Breast implants can have adverse effects on patients’ tissues and increase risks of reoperations or uncorrectable deformities if surgeons and patients make suboptimal preoperative choices and decisions. Excessively large implants can cause excessive stretch or thinning of patient tissues that is irreversible. When combined with normal effects of aging, thinning of soft tissues can compromise skin quality and reduce the efficacy of lifting procedures or other revisional procedures. Excessively projecting implants, especially when used in patients with tight envelopes (anterior pull skin stretch less than 2.5 cm), can cause atrophy of breast parenchyma that is irreversible and that compromises implant coverage and patients’ ability to nurse. No surgical procedure can improve the quality of tissues that have been compromised by excessively large or excessively projecting breast implants.
Essential principles to protect patients’ tissues and minimize reoperations, negative tissue consequences, and uncorrectable deformities long-term include (Table 2-4):
Table 2-4 Essentials to protect patient tissues from irreversible compromises and uncorrectable deformities
| Essential principle | Potential consequences if ignored |
|---|---|
| 1. Select implant pocket location to maximize available soft tissue coverage over all areas of the implant for the patient’s lifetime | Implant edge visibility, implant edge palpability, visible traction rippling |
| 2. Select base width of implant equal to or less than base width of patient’s parenchyma preop | Implant edge visibility, implant edge palpability, visible traction rippling |
| 3. Avoid excessively projecting breast implants | Parenchymal atrophy, chest wall deformities, excessive skin stretch and thinning, subcutaneous tissue thinning |
| 4. Avoid excessively large implants in all patients | Implant edge visibility, implant edge palpability, visible traction rippling, parenchymal atrophy, chest wall deformities, excessive skin stretch and thinning, subcutaneous tissue thinning |
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree