Procedure 2 Fasciotomy of the Upper Limb
Examination/Imaging
Clinical Examination
 Compartment syndrome is caused by increased pressure within the myofascial compartments leading to a decrease in blood flow. Nerves followed by muscle are most sensitive to ischemia and undergo irreversible changes within 6 to 8 hours. It is therefore important to decompress the fascial compartment by performing a fasciotomy and to restore tissue perfusion as soon as possible.
Compartment syndrome is caused by increased pressure within the myofascial compartments leading to a decrease in blood flow. Nerves followed by muscle are most sensitive to ischemia and undergo irreversible changes within 6 to 8 hours. It is therefore important to decompress the fascial compartment by performing a fasciotomy and to restore tissue perfusion as soon as possible.
 Compartment syndrome is a clinical diagnosis based on the features of ischemia of nerve (paresthesia, pain, and paralysis), muscle (pain on passive stretch), and vessel (pallor and pulselessness). All features may not be present in every patient, and a diagnosis is made based on the overall clinical scenario.
Compartment syndrome is a clinical diagnosis based on the features of ischemia of nerve (paresthesia, pain, and paralysis), muscle (pain on passive stretch), and vessel (pallor and pulselessness). All features may not be present in every patient, and a diagnosis is made based on the overall clinical scenario.
 A prophylactic fasciotomy should be performed in all major limb replantations/revascularizations irrespective of the clinical appearance of the limb at the end of the procedure (Fig. 2-4). The limb is insensate and becomes progressively swollen as a result of diminished venous return and ischemia reperfusion injury. When a fasciotomy is not performed, the arterial inflow can be compromised, leading to failure of the replantation.
A prophylactic fasciotomy should be performed in all major limb replantations/revascularizations irrespective of the clinical appearance of the limb at the end of the procedure (Fig. 2-4). The limb is insensate and becomes progressively swollen as a result of diminished venous return and ischemia reperfusion injury. When a fasciotomy is not performed, the arterial inflow can be compromised, leading to failure of the replantation.
Investigations
 No investigations are required if a diagnosis of compartment syndrome is clinically apparent. Some laboratory studies (complete blood count, prothrombin time, partial thromboplastin time, serum and urine myoglobin, and creatinine phosphokinase) and imaging studies (radiographs, Doppler, and arteriography) can be used to complement the clinical findings.
No investigations are required if a diagnosis of compartment syndrome is clinically apparent. Some laboratory studies (complete blood count, prothrombin time, partial thromboplastin time, serum and urine myoglobin, and creatinine phosphokinase) and imaging studies (radiographs, Doppler, and arteriography) can be used to complement the clinical findings.
 If a clinical diagnosis is equivocal, compartment pressure measurements should be obtained. We use a commercially available device (Stryker Intra-Compartmental Pressure Monitor) (Fig. 2-5). The normal tissue pressure is 0 to 8 mm Hg. A fasciotomy is recommended if the tissue pressure is higher than 30 mm Hg. Close monitoring, repeated clinical examination, and serial measurement of compartment pressures may be required for pressure measurements between 20 and 30 mm Hg.
If a clinical diagnosis is equivocal, compartment pressure measurements should be obtained. We use a commercially available device (Stryker Intra-Compartmental Pressure Monitor) (Fig. 2-5). The normal tissue pressure is 0 to 8 mm Hg. A fasciotomy is recommended if the tissue pressure is higher than 30 mm Hg. Close monitoring, repeated clinical examination, and serial measurement of compartment pressures may be required for pressure measurements between 20 and 30 mm Hg.
Surgical Anatomy
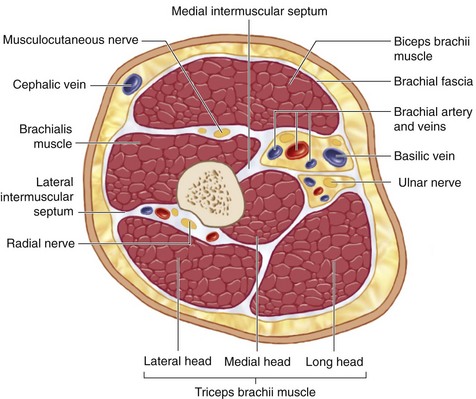
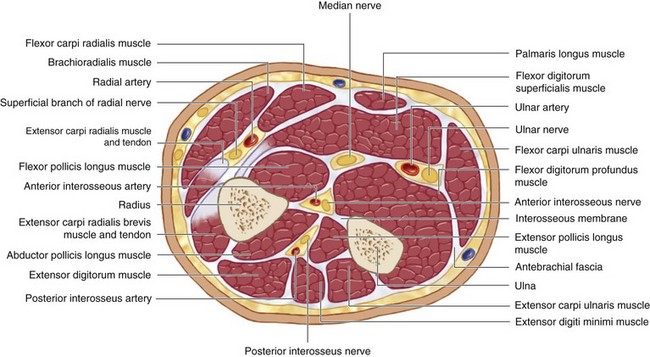
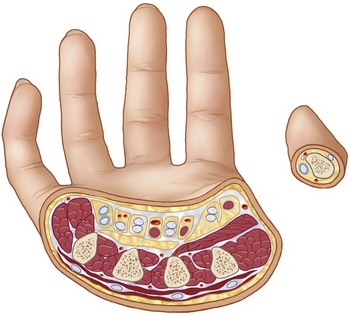
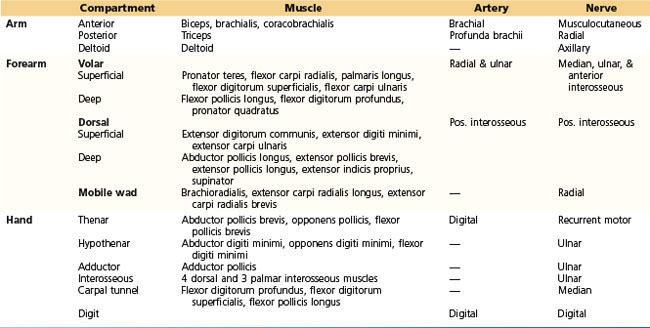
 The myofascial compartments of the upper extremity may be divided into compartments of the arm, forearm, and hand (Figs. 2-6, 2-7, and 2-8). The compartments and their contents are listed in Table 2-1.
The myofascial compartments of the upper extremity may be divided into compartments of the arm, forearm, and hand (Figs. 2-6, 2-7, and 2-8). The compartments and their contents are listed in Table 2-1.
 The brachial fascia of the arm is thin and poorly defined compared with the fascia of the forearm; therefore, development of increased pressure in the arm is less likely. Although a distinct fascial layer has not been defined in the hand, the glabrous skin overlying the thenar and hypothenar muscle compartments is relatively unyielding and serves as a constricting layer.
The brachial fascia of the arm is thin and poorly defined compared with the fascia of the forearm; therefore, development of increased pressure in the arm is less likely. Although a distinct fascial layer has not been defined in the hand, the glabrous skin overlying the thenar and hypothenar muscle compartments is relatively unyielding and serves as a constricting layer.
Positioning
 The procedure is performed under tourniquet control and regional or general anesthesia. The patient is positioned supine with the affected extremity on a hand table. A fasciotomy is usually done at the end of major limb replantation, and a tourniquet is not used in this situation. An emergency escharotomy may be done at the bedside for a circumferential third-degree burn because such a burn is not painful.
The procedure is performed under tourniquet control and regional or general anesthesia. The patient is positioned supine with the affected extremity on a hand table. A fasciotomy is usually done at the end of major limb replantation, and a tourniquet is not used in this situation. An emergency escharotomy may be done at the bedside for a circumferential third-degree burn because such a burn is not painful.
Exposures
Hand
 The carpal tunnel is decompressed by a single incision between the thenar and hypothenar muscles in line with the third web space (Fig. 2-9).
The carpal tunnel is decompressed by a single incision between the thenar and hypothenar muscles in line with the third web space (Fig. 2-9).
 The thenar compartment is decompressed by an oblique longitudinal incision along the radial margin of the thenar eminence (see Fig. 2-9).
The thenar compartment is decompressed by an oblique longitudinal incision along the radial margin of the thenar eminence (see Fig. 2-9).
 The hypothenar compartment is released via a longitudinal incision along the ulnar aspect of the palm (see Fig. 2-9).
The hypothenar compartment is released via a longitudinal incision along the ulnar aspect of the palm (see Fig. 2-9).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree