Procedure 19 Tendon Transfers for Ulnar Nerve Palsy
![]() See Video 15: Tendon Transfers for High Median and Ulnar Nerve Palsy
See Video 15: Tendon Transfers for High Median and Ulnar Nerve Palsy
Indications
 Delayed presentation (>1 year) of an ulnar nerve laceration
Delayed presentation (>1 year) of an ulnar nerve laceration
 Failed motor recovery after repair/reconstruction of the ulnar nerve
Failed motor recovery after repair/reconstruction of the ulnar nerve
 Failed motor recovery after release of ulnar nerve compression at Guyon canal or cubital tunnel
Failed motor recovery after release of ulnar nerve compression at Guyon canal or cubital tunnel
 Persistent motor weakness after completion of drug therapy in Hansen disease (leprosy)
Persistent motor weakness after completion of drug therapy in Hansen disease (leprosy)
 Neurologic disorders (for example, Charcot-Marie-Tooth disease, syringomyelia)
Neurologic disorders (for example, Charcot-Marie-Tooth disease, syringomyelia)
Examination/Imaging
Clinical Examination
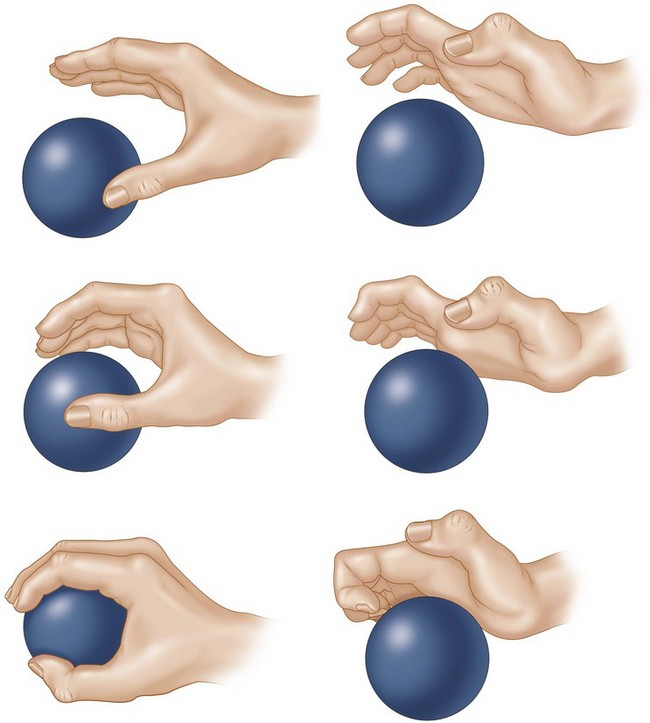
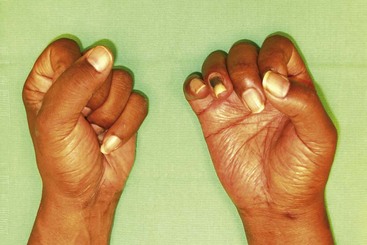
 Functional deficit: The loss of function in ulnar nerve palsy results from the claw deformity, which causes an abnormal pattern of finger flexion, weak thumb key pinch, small finger abduction deformity, and loss of ring and small finger distal interphalangeal (DIP) joint flexion (Fig. 19-1). However, these problems may not be functionally disabling in all patients, and some may require correction of only one aspect. It is important to determine this and then to set a sequence for the appropriate corrective procedures. It is better to correct the lack of DIP joint flexion first, followed by transfers for restoring thumb key pinch, and finally correction of the claw deformity because it is difficult to establish appropriate intrinsic plus posture of the hand.
Functional deficit: The loss of function in ulnar nerve palsy results from the claw deformity, which causes an abnormal pattern of finger flexion, weak thumb key pinch, small finger abduction deformity, and loss of ring and small finger distal interphalangeal (DIP) joint flexion (Fig. 19-1). However, these problems may not be functionally disabling in all patients, and some may require correction of only one aspect. It is important to determine this and then to set a sequence for the appropriate corrective procedures. It is better to correct the lack of DIP joint flexion first, followed by transfers for restoring thumb key pinch, and finally correction of the claw deformity because it is difficult to establish appropriate intrinsic plus posture of the hand.
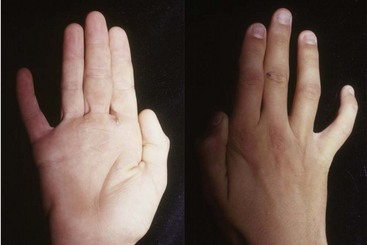
 Sensation: It is important to document the level of sensation in the thumb and the fingers preoperatively. Loss of sensation on the dorsoulnar aspect of the hand, which is innervated by the dorsal branch of ulnar nerve, can help differentiate a high ulnar nerve lesion (e.g., cubital tunnel compression) from a low ulnar nerve lesion (e.g., Guyon canal compression), which should have preserved sensation over the dorsal-ulnar hand (Fig. 19-7).
Sensation: It is important to document the level of sensation in the thumb and the fingers preoperatively. Loss of sensation on the dorsoulnar aspect of the hand, which is innervated by the dorsal branch of ulnar nerve, can help differentiate a high ulnar nerve lesion (e.g., cubital tunnel compression) from a low ulnar nerve lesion (e.g., Guyon canal compression), which should have preserved sensation over the dorsal-ulnar hand (Fig. 19-7).
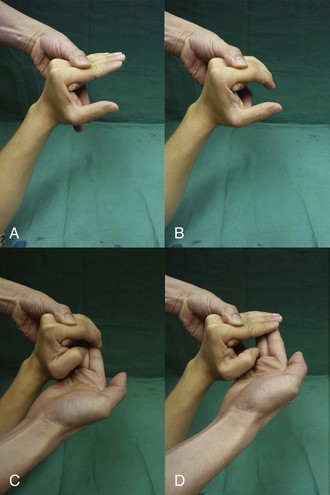
 Joints: To achieve a good result from the tendon transfer, patients must have good passive range of motion at the IP and the MCP joints. The most important aspect of assessment of an ulnar nerve palsy is determining whether the patient can extend the PIP joint with the examiner correcting the MCP joint hyperextension (Bouvier maneuver) (Fig. 19-8).
Joints: To achieve a good result from the tendon transfer, patients must have good passive range of motion at the IP and the MCP joints. The most important aspect of assessment of an ulnar nerve palsy is determining whether the patient can extend the PIP joint with the examiner correcting the MCP joint hyperextension (Bouvier maneuver) (Fig. 19-8).
 Selection of motor: We use a static procedure (MCP joint volar plate advancement) for correction of the claw deformity in patients who are able to achieve full active extension of the PIP joint. In patients unable to achieve full PIP joint extension, we use a dynamic transfer and prefer the long or ring finger FDS as a motor. We prefer to use the ring finger FDS in low ulnar nerve palsy because the FDS is important for chuck grip, which is predominantly a function of the thumb and index and long fingers. In patients with high ulnar nerve palsy with a weak or absent FDP to the ring finger, the FDS remains the only flexor of the ring finger, and it is prudent to use the long finger FDS. Other motors that have been described include the extensor indicis proprius (EIP) and EDM (both have insufficient length, resulting in excessive tension of the extensor apparatus), wrist flexors (flexor carpi radialis [FCR], palmaris longus [PL]), and wrist extensors (extensor carpi radialis longus [ECRL], extensor carpi radialis brevis [ECRB]). (All need a tendon graft.) We use the ECRB lengthened with a PL tendon graft as the motor for restoring thumb pinch. Other motors that have been described include the brachioradialis, ECRL, extensor carpi ulnaris (ECU), EIP, and FDS.
Selection of motor: We use a static procedure (MCP joint volar plate advancement) for correction of the claw deformity in patients who are able to achieve full active extension of the PIP joint. In patients unable to achieve full PIP joint extension, we use a dynamic transfer and prefer the long or ring finger FDS as a motor. We prefer to use the ring finger FDS in low ulnar nerve palsy because the FDS is important for chuck grip, which is predominantly a function of the thumb and index and long fingers. In patients with high ulnar nerve palsy with a weak or absent FDP to the ring finger, the FDS remains the only flexor of the ring finger, and it is prudent to use the long finger FDS. Other motors that have been described include the extensor indicis proprius (EIP) and EDM (both have insufficient length, resulting in excessive tension of the extensor apparatus), wrist flexors (flexor carpi radialis [FCR], palmaris longus [PL]), and wrist extensors (extensor carpi radialis longus [ECRL], extensor carpi radialis brevis [ECRB]). (All need a tendon graft.) We use the ECRB lengthened with a PL tendon graft as the motor for restoring thumb pinch. Other motors that have been described include the brachioradialis, ECRL, extensor carpi ulnaris (ECU), EIP, and FDS.
Surgical Anatomy
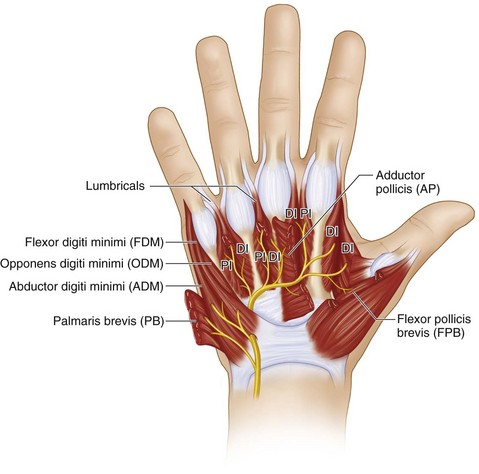
 The muscles affected after low ulnar nerve palsy are the four hypothenar muscles (abductor digitorum minimus [ADM], flexor digitorum minimus [FDM], opponens digitorum minimus [ODM], and palmaris brevis [PB]), seven interossei muscles (four dorsal and three palmar), third and fourth lumbricals, and two thenar muscles (adductor pollicis [AP] and the deep head of the flexor pollicis brevis [FPB]). All these muscles are innervated by the deep motor branch of the ulnar nerve (Fig. 19-10).
The muscles affected after low ulnar nerve palsy are the four hypothenar muscles (abductor digitorum minimus [ADM], flexor digitorum minimus [FDM], opponens digitorum minimus [ODM], and palmaris brevis [PB]), seven interossei muscles (four dorsal and three palmar), third and fourth lumbricals, and two thenar muscles (adductor pollicis [AP] and the deep head of the flexor pollicis brevis [FPB]). All these muscles are innervated by the deep motor branch of the ulnar nerve (Fig. 19-10).
 In high ulnar nerve palsy, the flexor carpi ulnaris (FCU) and the ulnar half of the FDP (ring and small fingers) are affected in addition to the muscles listed earlier.
In high ulnar nerve palsy, the flexor carpi ulnaris (FCU) and the ulnar half of the FDP (ring and small fingers) are affected in addition to the muscles listed earlier.
Procedure 1—Static Correction of Claw Deformity with an MCP Joint Volar Plate Advancement
Exposures
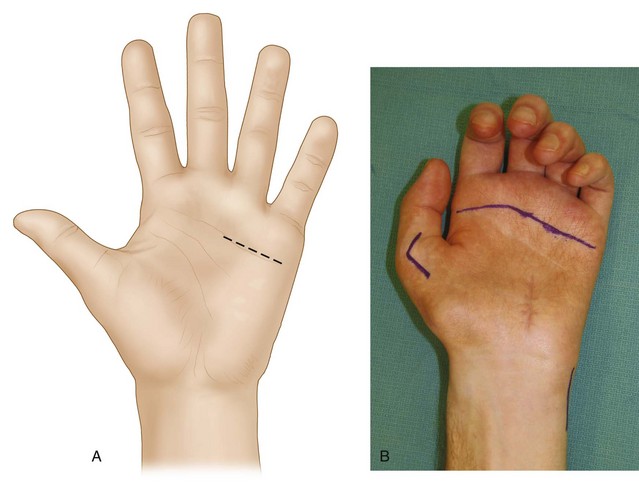
 A 3-cm transverse incision is made in line with the distal palmar crease overlying the ring and small finger MCP joints (Fig.19-11A and B).
A 3-cm transverse incision is made in line with the distal palmar crease overlying the ring and small finger MCP joints (Fig.19-11A and B).
 The skin and subcutaneous fat are dissected, and common digital neurovascular bundles are identified and protected.
The skin and subcutaneous fat are dissected, and common digital neurovascular bundles are identified and protected.
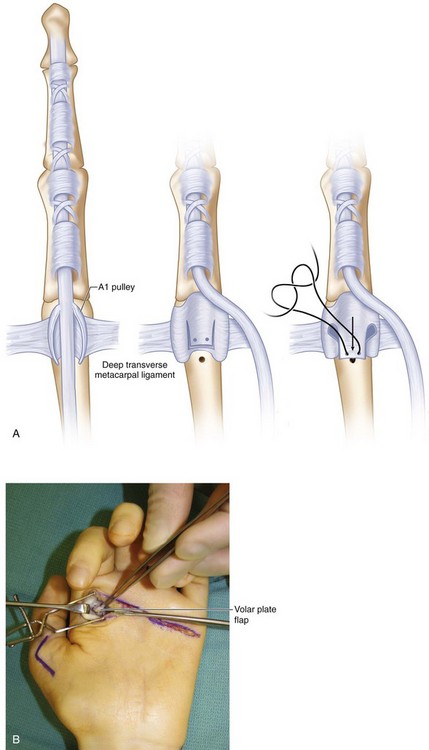
 The flexor tendon sheaths of the ring and small fingers are identified, and the A1 pulley is exposed (Fig. 19-12).
The flexor tendon sheaths of the ring and small fingers are identified, and the A1 pulley is exposed (Fig. 19-12).
Procedure
Step 1
 The A1 pulley of each finger is completely divided and the flexor tendons retracted to expose the volar plate of the MCP joint (Fig. 19-13).
The A1 pulley of each finger is completely divided and the flexor tendons retracted to expose the volar plate of the MCP joint (Fig. 19-13).
Step 3
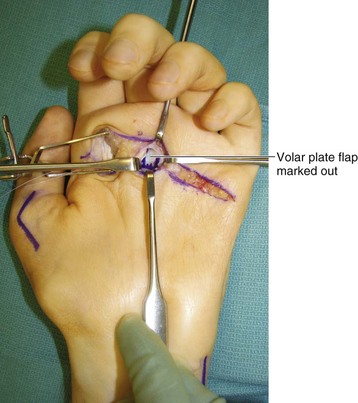
 A distally based flap of the volar plate is created by making two parallel longitudinal incisions and releasing the proximal attachment over the head of the metacarpal (Fig. 19-14A and B).
A distally based flap of the volar plate is created by making two parallel longitudinal incisions and releasing the proximal attachment over the head of the metacarpal (Fig. 19-14A and B).
Step 4
 A mini-Mitek bone anchor suture is inserted on the palmar surface of the neck of the metacarpal (Fig. 19-15).
A mini-Mitek bone anchor suture is inserted on the palmar surface of the neck of the metacarpal (Fig. 19-15).