Chapter 19 Glandular Ptotic and Constricted Lower Pole Breasts
Achieving optimal augmentation results in breasts with glandular ptosis or a constricted lower pole requires that surgeons have a detailed knowledge of the anatomy and implant–soft tissue dynamics that are unique to these two breast types. Suboptimal outcomes occur frequently following augmentation of these breast types when surgeons apply routine augmentation principles to operative planning and implant and technique selection.
Requirements for Optimal Correction in Glandular Ptotic and Constricted Lower Pole Breasts
Glandular ptotic breasts and constricted lower pole breasts have significant anatomic differences, but optimal correction of both deformities with augmentation has common requirements (Table 19-1): (1) surgical correction of the anatomic layer(s) that produce the deformity, (2) selection of implant type and size that allows the surgeon to control distribution of fill and pressure that the implant exerts on adjacent tissues, (3) redistribution or repositioning of tissue relative to the implant, (4) tissue layer interface control, (5) precise intraoperative control of implant pocket dimensions, and (6) precise positioning of the implant within the soft tissue pocket.
Table 19-1 Requirements for correction of glandular ptotic and constricted lower pole breasts
Categorizing Breast Ptosis
The most commonly recognized classification of breast ptosis was first published in 1976 by Paula Regnault.1 This classification and subsequent modifications of the classification, while useful for many years, share common deficiencies that confuse many surgeons and contribute to selection of suboptimal surgical techniques for correction.
All current classifications of breast ptosis that relate the position of the nipple to the level of the projected inframammary fold are extremely subjective, non-quantitative, and subject to a wide range of surgeon interpretations. Absent measurements to quantify the amount of skin in the lower pole of the breast (nipple-to-inframammary fold distance measured under maximal stretch2,3) surgeons make judgments and select techniques for correction by viewing the breast laterally in photographs or in the clinical setting, and subjectively assign a level of the nipple relative to the level of the projected inframammary fold anteriorly. This method, though widely used, is exceedingly inaccurate and subject to a wide range of variables. When surgeons use this method, and then select a surgical technique for correction of the deformity based on a subjective and relatively inaccurate and inconsistent visual estimation, it is not surprising that a large number of suboptimal corrections and subsequent revision or reoperation procedures occur.
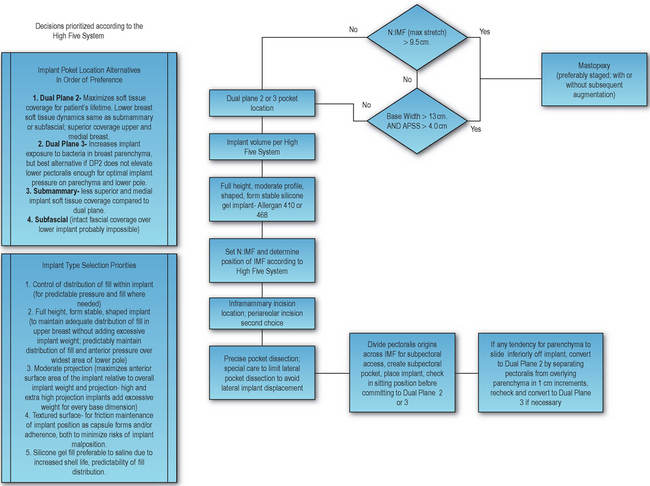
Surgeons should recognize the critical importance of establishing quantitative guidelines to define degrees of breast ptosis that may be correctable by an implant alone versus degrees of ptosis that require mastopexy, with or without augmentation. The single quantitative factor that best defines whether a breast implant alone may correct a ptosis deformity is nipple-to-inframammary fold distance measured under maximal stretch (N:IMFmax stretch). When N:IMF exceeds 9.5 cm and/or breast width exceeds 13 cm, surgeons should not attempt correction of the ptosis deformity with an implant alone.2,3Figure 19-1 emphasizes the need to strongly consider mastopexy when N:IMF measured under maximal stretch exceeds 9.5–10 cm.
The degree to which an implant is likely to accomplish optimal correction of a sagging breast is determined by the amount of skin in the lower pole of the breast (N:IMFmax stretch) and the amount of filler material required to optimally and fully expand the lower pole. The longer the N:IMF measurement, the wider the breast, and the less parenchyma present preoperatively, the greater the implant volume required to optimally expand the skin envelope and create adequate projection to optimally correct the deformity.
Using quantitative measurements to define limits for augmentation alone versus mastopexy (with or without an implant) eliminates the inherent inaccuracies of subjective judgments of nipple position relative to the inframammary fold.2,3 Ptosis deformities in which the nipple–areola complex is located 1–1.5 cm below the level of the projected inframammary fold, indicate formal mastopexy according to most systems that classify ptosis using nipple position relative to the projected inframammary fold. A subset of these cases, however, has a low nipple position relative to the inframammary fold, but may have a N:IMF of 8.0–9.0 cm or less, indicating that the deformity is likely correctable by implant alone, avoiding unnecessary tradeoffs and risks of mastopexy. In subjective terms, a patient can have an “empty” breast that appears “sagging”, but if N:IMF is 9.5 cm or less and base width is 13 cm or less, the “emptiness” factor that is causing the sagging appearance can likely be corrected with an implant alone. When N:IMF and BW exceed the previously defined parameters, the volume of implant required to optimally expand the envelope for optimal correction becomes excessive, often exceeding 400–500 cc, and surgeons should counsel the patient regarding the tradeoffs of excessively large, low breasts compared to the tradeoffs of mastopexy.
The Glandular Ptotic Breast
The generic term “glandular ptotic” is inherently subjective and poorly defines one segment of a range of breast ptosis deformities. Three components must exist simultaneously to create a glandular ptotic or ptotic breast: (1) weakness or stretch of soft tissue attachments at the parenchyma–muscle interface, (2) a mobile mass of parenchyma, and (3) excess skin (by stretch) in the lower pole envelope to allow descent of the parenchymal mass. Descent of the nipple–areola complex is a separate component, and the extent to which the complex descends depends on the degree of stretch in the skin of the upper breast envelope.
Criteria for Augmentation without Mastopexy for Correcting the Glandular Ptotic Breast
Theoretically, the nipple–areola complex (NAC) in the glandular ptotic breast is located at or above the level of the anteriorly projected inframammary fold (Figure 19-2). The position of the nipple with respect to the projected inframammary fold, as previously discussed, does not accurately define the variables that affect correction of this type of breast deformity. For example, the nipple can appear to be below the level of the projected inframammary fold, but N:IMF may be only 8–8.5 cm if minimal parenchyma is present. This degree of lower pole stretched envelope certainly does not require a mastopexy for optimal fill and aesthetic correction. A 300 cc breast implant in conjunction with a dual plane type 2 pocket dissection predictably corrects this deformity without subjecting the patient to all of the tradeoffs and risks of a mastopexy.
Analyzing this type of deformity using the High Five™ System3 quickly identifies and quantifies indications for augmentation alone or mastopexy (Table 19-2).
Table 19-2 Applying the High Five™ System to determine the necessity of mastopexy or augmentation alone
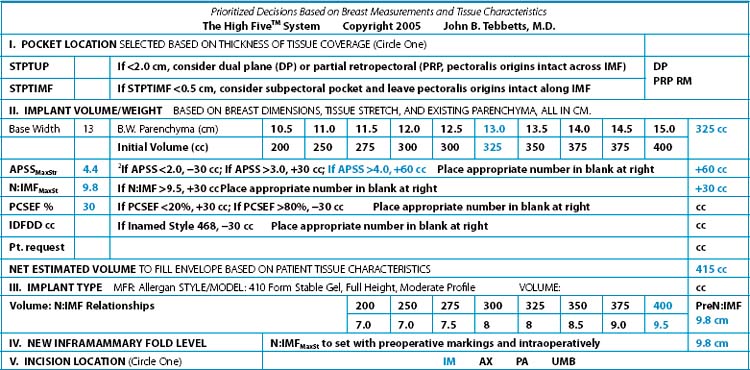
According to the system, a 13 cm base width requires 325 cc volume for optimal fill. If anterior pull skin stretch (APSS) exceeds 3 cm, as it virtually always does with a stretched envelope (glandular ptotic) breast, the system recommends adding 30 cc to the starting volume for a total of 355 cc. If APSS exceeds 4 cm, an additional 30 cc or a 385 cc volume would be required. Finally, if N:IMF exceeds 9.5 cm, the system recommends adding another 30 cc for a total of 415 cc. While this size implant may adequately expand the lower pole envelope and improve appearance, even this significant volume may not adequately fill the upper pole of the breast. Regardless, this weight implant in an envelope that has already proved it stretches excessively as a result of genetics, aging, or pregnancy, is unlikely to sustain a satisfactory aesthetic result at best, and at worst could quickly develop a “rock in a sock” appearance of a much larger breast that appears low on the torso. Rationale for implant type selection and level of the inframammary fold in this example are discussed later in this chapter.
Informed Consent Considerations for Patients with Glandular Ptosis
Implant–Soft Tissue Dynamics in the Glandular Ptotic Breast
The key to success or failure in treating glandular ptotic breasts with augmentation alone is the posterior interface of the parenchyma with either the anterior capsule in submammary, subfascial, or dual plane4 2 augmentations, or the parenchyma–muscle interface if the surgeon places the implant subpectorally. Traditional subpectoral augmentation, leaving pectoralis origins intact along the inframammary fold, is almost predictably doomed to failure, because the surgeon has not addressed the weak attachments at the parenchyma–muscle interface that allowed the glandular tissue to slide inferiorly to create the preoperative deformity of glandular ptosis. A traditional subpectoral augmentation almost predictably results in the parenchyma sliding inferiorly off the pectoralis and underlying implant to create a “double bubble” deformity in the breast lower pole. Correction of the “double bubble” deformity requires either: (1) a conversion to a dual plane4 2 pocket with division of pectoralis origins along the inframammary fold and separation of parenchyma–muscle attachments to allow superomedial rotation of the lower pectoralis edge (this option optimizes soft tissue coverage medially and superiorly), or (2) conversion to a submammary or subfascial pocket which does not provide as good long-term soft tissue coverage medially and superiorly. With either conversion option, radial scoring of any palpable banding transversely at the level of the preoperative inframammary fold is often necessary for optimal release and correction.
Regardless of whether a surgeon chooses to augment the glandular ptotic patient using a submammary, subfascial, or dual plane4 2 pocket, the surgeon must realize and inform the patient that the glandular tissue may unavoidably slide downward off the anterior surface of the anterior capsule that forms around the implant. No type of implant, regardless of surface characteristics, shape, or profile/projection can predictably assure that glandular tissue will not continue to slide inferiorly off the capsule. If inferior descent of glandular tissue occurs despite a properly performed dual plane4 2 or 3 pocket, or following submammary or subfascial placement, correction will require formal mastopexy to remove skin from the lower envelope (excess skin envelope is present by definition if the parenchymal mass descends, and the excess is both vertical and horizontal). Surgeons should be especially cautious when attempting to correct this secondary deformity, and assure adequate removal of skin vertically in the breast lower pole. Mastopexy techniques that limit scars to periareolar and vertical usually fail to correct this secondary deformity because they fail to remove adequate skin from the breast lower pole, choosing to rotate excess skin upward to minimize scar length.
Regardless of whether a surgeon chooses to augment the glandular ptotic patient using a submammary, subfascial, or dual plane4 2 pocket, the surgeon must realize and inform the patient that the glandular tissue may unavoidably slide downward off the anterior surface of the anterior capsule that forms around the implant
Surgical Correction of the Glandular Ptotic Breast
Figure 19-3 is a flowchart that summarizes alternatives for surgical correction of the glandular ptotic breast.
Provided that N:IMF is 9.5 cm or less, and base width 13 cm or less, a dual plane type 2 pocket dissection and a full height, form stable, moderate profile implant selected according to the High Five™ system3 provides excellent correction and optimal long-term outcomes in a majority of cases. Submammary and subfascial pocket locations are not best for the patient long-term, because neither provides maximal soft tissue coverage medially and superiorly for the patient’s lifetime, risking reoperations or uncorrectable deformities such as visible implant edges and traction rippling medially or superiorly. A dual plane type 2 or 3 pocket provides optimal correction and optimal long-term soft tissue coverage for most areas of a glandular ptotic breast. Disrupting the parenchyma–muscle interface by using the dual plane4 2 technique is critically important to minimize risks of the parenchyma sliding inferiorly off the muscle. With the dual plane 2, the inferior cut edge of the pectoralis moves superiorly by superomedial rotation to the level of the nipple or lower border of the areola. Details of technique are included in Chapters 8 and 11.
An inframammary incision approach provides the most exposure, control, and versatility for adjusting the position of the pectoralis for a dual plane4 2 or 3 pocket
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree