Chapter 18 Wound Healing, Capsular Contracture, and Tissue Stretch: Factors Surgeon and Patient Cannot Control
Surgeon decisions and technical execution largely determine patient outcomes in breast augmentation, but neither surgeons nor patients can control wound healing mechanisms and neither can predict or control tissue stretch following augmentation. Wound healing mechanisms and tissue stretch may seem unrelated, but these topics impact outcomes in two distinct ways: (1) wound healing mechanisms during capsule formation and contraction directly impact the degree of lower pole soft tissue stretch that occurs following augmentation, and (2) wound healing and tissue stretch mechanisms determine incidence of several causes of reoperations, including infection, capsular contracture, implant malposition or displacement, and lower pole stretch deformities.
The Role of Patient Education in Managing Postoperative Challenges
During the preoperative patient education process, surgeons should provide patients with written information that describes specific areas of wound healing and tissue stretch that are not controllable by surgeon or patient. After reading the written information, patients should receive verbal reinforcement of key concepts and have an opportunity to ask questions about factors that surgeon and patient cannot control. Before surgery, patients should acknowledge their understanding and acceptance of factors that surgeon and patient cannot control, and acknowledge the problems, reoperations, costs, and risks that are associated with these uncontrollable mechanisms in clearly written informed consent documents.
Educating the Patient About Factors the Surgeon Cannot Control
The following content is excerpted from a preoperative patient education DVD and accompanying document entitled “My Preferences and Information I Fully Understand and Accept” that are components from a staged, repetitive, and comprehensive system for augmentation patient education that is peer reviewed and published in the journal Plastic and Reconstructive Surgery.1 As the DVD presents information in stages, the program pauses at intervals to allow the patient to read the accompanying printed document and document an understanding and acceptance of the information. Video content from the patient education program and the accompanying document are included in the Resources folder on the DVDs that accompany this book.
Before I examine you, I want to discuss with you three specific areas that concern me the most, because they are areas that I cannot totally predict or control: (1) whether or not you will develop infection, (2) how much the capsule you form around your implants will tighten and how that capsule may affect the appearance, softness, or feeling in your breasts, and (3) how much your tissues will stretch in response to your implants. Let’s talk about each area separately, but first, *If you are at a computer equipped to interact with the DVD, please confirm your understanding of this information by placing your signature in the box onscreen. Next, on your paper informed consent document, carefully read and initial items 15 and 16. When you have completed this portion of the program, please click on the Next Topic button on the screen.
Document used by the patient while watching the video:
Once implants are removed, infection usually subsides with the help of antibiotics over a 1–3 week period, but the tissues of the breast require at least 3 months to soften and heal. The more aggressive the infection, the greater the risk of internal or external scarring that can leave permanent deformities.
Every patient who has an augmentation forms capsules around her implants. Unfortunately, there are no tests we can perform on you prior to surgery to predict whether the capsules you form will tighten excessively and cause deformities. If we could predict that you are likely to form an excessively tight capsule, we would advise you not to have an augmentation, but unfortunately we cannot predict or control how your body heals and how much your capsule will tighten.
If any of these problems caused by the capsule are mild to moderate, I may not recommend a reoperation. When the problems are mild, your body is sending us a message that your healing mechanisms tend to form tight capsules. If we reoperate, we are not changing your body’s healing mechanisms, and you might form an even worse capsule with worse deformities than you already have. On the other hand, if the deformities are severe, and I have to be the judge of that, we may need to reoperate. Our experience has taught us that regardless of how rapidly a capsule tightens, we should not reoperate on that capsule until at least 6 months following the initial surgery. During that time, the capsule is forming and maturing, and if we interrupt that process, recurrence of the excessively tight capsule is almost certain.
If you develop a deformity from unpredictable or excessive stretch of your tissues, surgical correction of those stretch deformities is unpredictable at best, because we are operating on the same tissues that have already demonstrated that they will stretch excessively. We can change to a smaller implant to decrease weight, but the stitches placed internally to close off the excess pocket and reposition the implant may not hold in the thin tissues against the weight of even a smaller implant, and the stretch deformity may recur. If a stretch deformity recurs after a surgery to attempt to correct it, we will usually recommend implant removal without replacement to avoid even further stretch and thinning of your tissues that could cause permanent uncorrectable deformities.
Surgeon Discussion of Wound Healing and Tissue Stretch Factors
The following paraphrases the conversation that the author has with patients during the surgeon consultation:
Distinguishing Inferior Pocket Closure from Capsular Contracture
After every breast augmentation, some degree of dead space exists around the implant, regardless of the precision of pocket dissection. Small amounts of serous or serosanguinous fluid accumulate immediately postoperatively, even if a surgeon places drains which are unnecessary in primary augmentation. Wound healing mechanisms attempt to close dead space, but the amount and location of closure varies substantially from one case to another or from one breast to the other in the same patient.
The most common area of fluid accumulation is the inferior pocket sulcus along the inframammary fold. Small amounts of fluid accumulate in this area regardless of whether a surgeon uses a drain. Immediately postoperatively, a triangular dead space exists in the inferior-most portion of the pocket along the inframammary fold (Figure 18-1, A) because the implant does not completely fill the lower pocket due to pressure of overlying soft tissues. The larger or more projecting an implant, the larger the dead space along the inframammary fold, but some dead space exists in this area regardless of implant type, size, or pocket location (Figure 18-1, B).
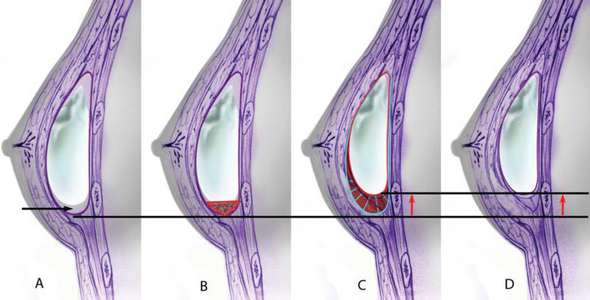
Figure 18-1 A Dead space exists in the implant pocket inferior to the implant after every breast augmentation.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






