Procedure 18 Tendon Transfers for Carpal Tunnel Syndrome
![]() See Video 14: Tendon Transfer for Anterior Interosseous Nerve Palsy (FDS to FPL)
See Video 14: Tendon Transfer for Anterior Interosseous Nerve Palsy (FDS to FPL)
Examination/Imaging
Clinical Examination
 Sensation: It is important to document the level of sensation in the thumb and fingers preoperatively. Patients may also have diminished sensation in the ulnar nerve distribution. The potential functional benefit of a tendon transfer will be diminished in a patient with sensory loss, and these patients must be counseled about the likely poorer outcome after surgery.
Sensation: It is important to document the level of sensation in the thumb and fingers preoperatively. Patients may also have diminished sensation in the ulnar nerve distribution. The potential functional benefit of a tendon transfer will be diminished in a patient with sensory loss, and these patients must be counseled about the likely poorer outcome after surgery.
 Joints: To get a good result from the tendon transfer, patients must have good passive range of motion at the thumb metacarpophalangeal (MCP) joint and the thumb carpometacarpal (CMC) joint. It is not uncommon for patients to have basal joint arthritis with a supination and adduction deformity of the thumb and first web-space contracture. This should be addressed before a tendon transfer is considered.
Joints: To get a good result from the tendon transfer, patients must have good passive range of motion at the thumb metacarpophalangeal (MCP) joint and the thumb carpometacarpal (CMC) joint. It is not uncommon for patients to have basal joint arthritis with a supination and adduction deformity of the thumb and first web-space contracture. This should be addressed before a tendon transfer is considered.
 Motor: Many motors have been described for opponensplasty. Our first preference is the palmaris longus (PL) followed by the extensor indicis proprius (EIP), if the PL is absent. We rarely use the flexor digitorum superficialis (FDS) of the ring finger because of the greater morbidity (weakening the power grip, risk for proximal interphalangeal [PIP] joint flexion contracture, swan-neck deformity) and because the soft tissue pulley attenuates over time. Although the tension fraction of PL (1.2%) and EIP (1%) is theoretically less than the combined tension fraction of abductor pollicis brevis (APB) (1.1%) and opponens pollicis (OP) (1.9%), the transfer only needs enough strength to position the thumb in abduction.
Motor: Many motors have been described for opponensplasty. Our first preference is the palmaris longus (PL) followed by the extensor indicis proprius (EIP), if the PL is absent. We rarely use the flexor digitorum superficialis (FDS) of the ring finger because of the greater morbidity (weakening the power grip, risk for proximal interphalangeal [PIP] joint flexion contracture, swan-neck deformity) and because the soft tissue pulley attenuates over time. Although the tension fraction of PL (1.2%) and EIP (1%) is theoretically less than the combined tension fraction of abductor pollicis brevis (APB) (1.1%) and opponens pollicis (OP) (1.9%), the transfer only needs enough strength to position the thumb in abduction.
 The transfer of the PL (Camitz transfer) is typically performed for an elderly patient with CTS and severe thenar atrophy. The Camitz transfer is considered a “freebie” procedure because the incision used for CTS can be extended to the wrist in a zigzag fashion to obtain the PL augmented by the palmar fascia to attach into the ABP insertion at the radial MCP joint. As with any freebie procedure, however, the direction of tendon pull is not in line with the APB muscle but rather is more parallel to the forearm, which does diminish the biomechanical construct of this tendon transfer procedure. For an elderly patient with modest functional requirements, this transfer does serve the purpose of restoring some abduction and will permit the patient to recover acceptable thumb function.
The transfer of the PL (Camitz transfer) is typically performed for an elderly patient with CTS and severe thenar atrophy. The Camitz transfer is considered a “freebie” procedure because the incision used for CTS can be extended to the wrist in a zigzag fashion to obtain the PL augmented by the palmar fascia to attach into the ABP insertion at the radial MCP joint. As with any freebie procedure, however, the direction of tendon pull is not in line with the APB muscle but rather is more parallel to the forearm, which does diminish the biomechanical construct of this tendon transfer procedure. For an elderly patient with modest functional requirements, this transfer does serve the purpose of restoring some abduction and will permit the patient to recover acceptable thumb function.
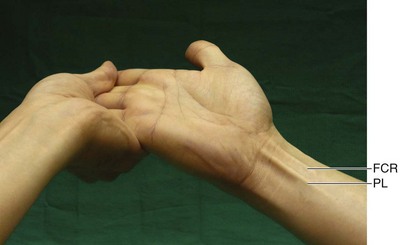
 We use the test described by Mishra to determine the presence of the PL. The traditional test described by Schaeffer requires the patient to abduct and oppose the thumb to the small finger and flex the wrist. A patient with thenar atrophy will find it difficult to do so. The Mishra test is performed by holding the patient’s wrist and fingers in hyperextension, while asking the patient to flex the wrist. This stretches the palmar aponeurosis and makes the PL taut when the patient attempts wrist flexion (Fig. 18-1).
We use the test described by Mishra to determine the presence of the PL. The traditional test described by Schaeffer requires the patient to abduct and oppose the thumb to the small finger and flex the wrist. A patient with thenar atrophy will find it difficult to do so. The Mishra test is performed by holding the patient’s wrist and fingers in hyperextension, while asking the patient to flex the wrist. This stretches the palmar aponeurosis and makes the PL taut when the patient attempts wrist flexion (Fig. 18-1).
Surgical Anatomy
 Thumb opposition is a complex movement produced by a combination of flexion, palmar abduction, and pronation and requires participation of both the MCP and CMC joints. The prime muscle of thumb opposition is believed to be the APB with contributions from the OP and flexor pollicis brevis (FPB).
Thumb opposition is a complex movement produced by a combination of flexion, palmar abduction, and pronation and requires participation of both the MCP and CMC joints. The prime muscle of thumb opposition is believed to be the APB with contributions from the OP and flexor pollicis brevis (FPB).
 The muscles affected after low median nerve palsy are the APB, OP, superficial head (radial head) of the FPB, and the radial two lumbricals (first and second). The first three muscles are innervated by the recurrent motor branch of the median nerve, whereas the latter two are innervated by the first and second common palmar digital nerve branch of the median nerve.
The muscles affected after low median nerve palsy are the APB, OP, superficial head (radial head) of the FPB, and the radial two lumbricals (first and second). The first three muscles are innervated by the recurrent motor branch of the median nerve, whereas the latter two are innervated by the first and second common palmar digital nerve branch of the median nerve.
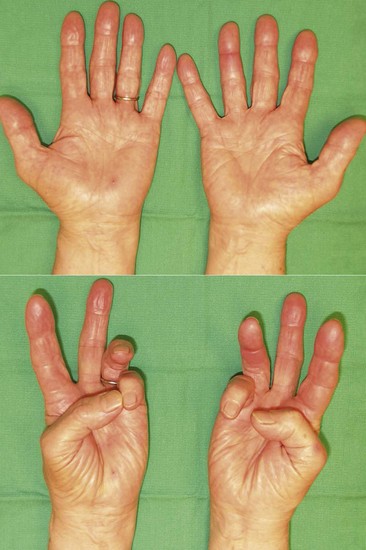
 Reasonable thumb abduction and opposition may be retained after isolated median nerve injury or severe carpal tunnel syndrome as a result of preserved ulnar nerve function (retained innervation of the deep head of the FPB and variability in thenar muscle innervation by connection between the ulnar and median nerves). Figure 18-2 shows the preoperative appearance of the hand with severe CST on the right. Note the thenar atrophy and inability to palmarly abduct the right thumb.
Reasonable thumb abduction and opposition may be retained after isolated median nerve injury or severe carpal tunnel syndrome as a result of preserved ulnar nerve function (retained innervation of the deep head of the FPB and variability in thenar muscle innervation by connection between the ulnar and median nerves). Figure 18-2 shows the preoperative appearance of the hand with severe CST on the right. Note the thenar atrophy and inability to palmarly abduct the right thumb.
 The midpalmar portion of the palmar aponeurosis has three layers: superficial longitudinal fibers, deeper transverse fibers, and deepest vertical fibers. Only the superficial longitudinal fascia is obtained in continuity with the PL to maximize the length of this tendon to reach the APB insertion.
The midpalmar portion of the palmar aponeurosis has three layers: superficial longitudinal fibers, deeper transverse fibers, and deepest vertical fibers. Only the superficial longitudinal fascia is obtained in continuity with the PL to maximize the length of this tendon to reach the APB insertion.
Positioning
 The procedure is performed under tourniquet control. It is usually performed under sedation and local anesthesia because this procedure is rather expedient and there is no need to take unnecessary anesthetic risk in elderly patients. The patient is positioned supine with the affected extremity on a hand table.
The procedure is performed under tourniquet control. It is usually performed under sedation and local anesthesia because this procedure is rather expedient and there is no need to take unnecessary anesthetic risk in elderly patients. The patient is positioned supine with the affected extremity on a hand table.