Chapter 15 Essentials to Achieve 24 Hour Recovery
Most informed patients considering breast augmentation want an optimal result with the shortest, most carefree recovery and the least risk of problems, reoperations, and costs in the future. Surgeons and breast implant manufacturers serve the patient and prioritize a commitment to continually deliver the best for the patient. The patient experience encompasses all aspects of education, perioperative care, and long-term outcome. An optimal patient experience requires surgeon commitment to continually optimize decisions and processes that determine outcomes.
The same decision processes and surgical techniques that deliver 24 hour recovery also deliver optimal long-term outcomes with low complication and reoperation rates1–6
Most plastic surgeons can develop a skill set to predictably deliver 24 hour return to normal activities following breast augmentation, provided they are willing and able to commit time and resources. Surgeons less than 5 years in practice have developed all of the necessary skills discussed in this chapter, and by implementing the processes detailed in this chapter and this book, predictably deliver 24 hour recovery. The same decision processes and surgical techniques that deliver 24 hour recovery also deliver optimal long-term outcomes with low complication and reoperation rates.1–6 In 1664 reported consecutive augmentations using inframammary, axillary, and periareolar incision approaches and submammary, partial retropectoral, and dual plane pockets, patients experienced an overall reoperation rate of less than 3% with up to 7 year followup.4,6,7 The incidence of other untoward occurrences in these combined series includes: capsular contracture Grades 3 and 4—0.7%, hematoma—0.2%, seroma—0.1%, infection—0.3%, implant deflations—0.8%, reoperations for implant malposition with anatomic implants—0.1%, and reoperations for size exchange—0.2%. The occurrence of visible wrinkling with the patient upright was zero by prioritizing tissue coverage based on quantitative tissue parameters2,3 and optimal surgical techniques.4,6 These data prove that the same factors that enable 24 hour recovery also optimize long-term outcomes by minimizing complications and reoperations.
This chapter summarizes and codifies essential information that is included in other chapters, and focuses on specific requirements to deliver a redefined level of care and recovery. These processes are derived from a 15 year focus on breast augmentation, using process engineering principles to analyze and refine processes in each of the following areas: patient education and informed consent;1 objective, quantitative preoperative tissue based assessment;2 defined decision making priorities and processes;3 surgical techniques and instrumentation;4–6 perioperative care and anesthesia; and postoperative care.5,6
The methodologies and processes that allow surgeons to deliver a redefined level of care are complementary. Seemingly insignificant aspects of one process contribute significantly to the efficacy of other processes. Other alternatives and processes may predictably enable over 85% of patients to be out to dinner the evening of surgery and 96% to return to full, normal activities within 24 hours,5,6 but other alternatives are not currently peer reviewed and published. Process engineering principles, motion and time study principles, and cause and effect analyses have provided invaluable tools that encouraged analysis and refinement of surgical processes from a perspective that is different compared to the “solution for problem” surgeon thought process that surgeons learn in an apprenticeship residency setting. Achieving 24 hour recovery is an excellent benchmark for the entire patient experience, because recovery is objective, and not subject to varying interpretations. Optimal recovery correlates directly with minimal complications, minimal reoperations, and optimal long-term outcomes.1–6
Achieving 24 hour recovery is an excellent benchmark for the entire patient experience, because recovery is objective, and not subject to varying interpretations. Optimal recovery correlates directly with minimal complications, minimal reoperations, and optimal long-term outcomes1–6
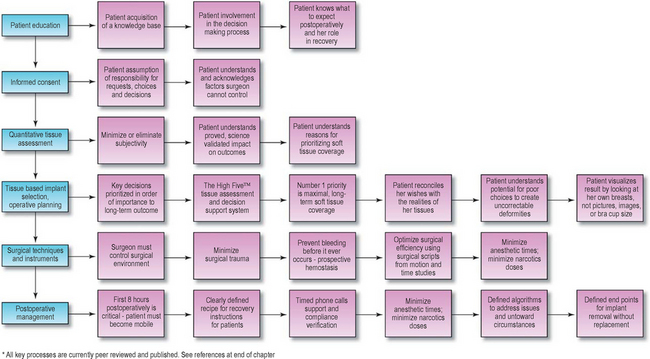
Other chapters in this book present the details of the processes that deliver 24 hour recovery and optimal long-term outcomes. This chapter summarizes the key elements that determine optimal recovery and outcomes. Table 15-1 summarizes the six key defined process categories and the individual processes in each category that are essential for surgeons to predictably deliver this level of patient recovery and outcome.
Table 15-1 Essential processes to achieve 24 hour recovery and optimal outcomes.
Patient Education and Informed Consent
Legally valid informed consent requires that patients make decisions. Optimal decisions require knowledge and decision support that provide patients factual information about all alternatives, and base patient and surgeon choices on proved decision processes.1,3 Optimal patient education is staged and repetitive,1 supports the patient in making decision, but requires that the patient ultimately makes choices and assumes documented responsibility for those choices.
Clearly defining what the patient and the surgeon cannot control is critically important during the patient education and informed consent process. Patients and surgeons cannot control two specific areas that can potentially produce untoward events or results postoperatively: wound healing (infection, capsular contracture), and tissue stretch (tissue stretch, thinning, and the resultant deformities). Understanding the decision parameters that minimize risks in these areas helps patients make better preoperative decisions, but patients must understand, accept, and take responsibility for the reality that neither patient nor surgeon can control the body’s mechanisms in these two areas. Methods and documentation to assure patient understanding of these important limitations are detailed in Chapter 3.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree