Chapter 14 Preoperative Care, Anesthesia, and Postoperative Care
Creating An Optimal Perioperative Environment
When surgeons can accomplish the requirements listed above, both the surgeons and the surgical facility can increase efficiency, profitability, and improve patient recovery by allocating two operating rooms for a single surgeon during a specific period (Figure 14-1). This system minimizes surgeon and personnel downtime, maximizes the surgical facility’s return on investment of personnel resources and facility resources, and encourages all team members to perform at a higher level. This system is only logical if surgeons have a reasonable case load of augmentations, and if the surgeon and surgeon’s personnel learn to manipulate patient scheduling to assure a minimum of three augmentations on any surgery day. The system fails miserably when surgeons want to perform one or two augmentations on a day, or during a block time.
Preoperative Care
Preoperative Preparations
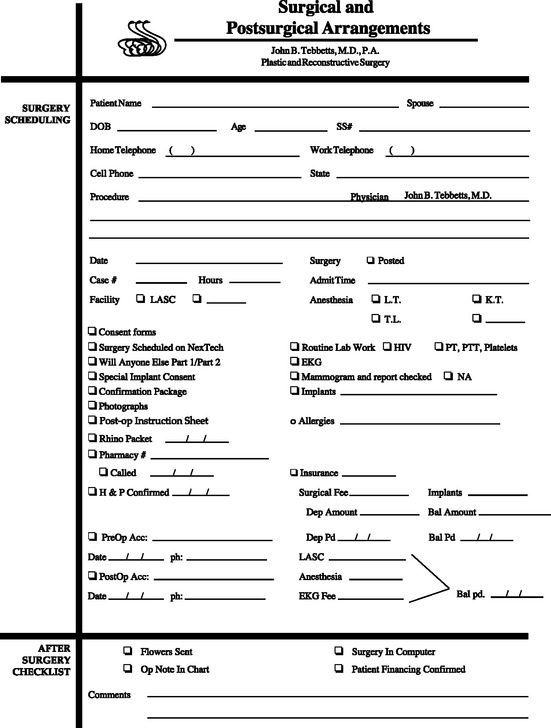
All of this information should be included in printed information to the patient and on a checklist that is immediately accessible to all surgeon personnel who might interact with the patient. A specific surgeon employee should be responsible for providing this information and placing a preoperative checklist (Table 14-1) on the front of the patient’s chart that provides instant information to all other personnel that interact with the patient. This document is available in the Resources folder on the DVDs that accompany this book.
Table 14-1 Surgical and postsurgical arrangements.
Patients must understand the critical importance of each of the following:
Arrival and Transfer to Surgical Holding
When the patient arrives at the surgery facility, personnel (ideally, personnel who know the patient) should be available to meet the patient and caregiver, and immediately accompany the patient to an area where the patient can change into a surgical gown (Figures 14-2, 14-3). All of the patient’s valuables should remain with the patient’s caregiver, and personnel should get a cell phone number for the caregiver or accompany the caregiver to an appropriate waiting area. Personnel should plan to have the caregiver available at the surgery center when the patient first enters the recovery room, so that personnel can review postoperative instructions with the caregiver and review them with the patient within the hour after the patient’s operation. In a 627 consecutive patient series of augmentation patients,1,2 using management protocols and surgical techniques included in this chapter, the average time from the start of the patient’s breast augmentation under general anesthesia to discharge with an ASPAN3 score of 10 was 78 minutes. Continuing to monitor and improve proved processes has further reduced perioperative recovery times and time to discharge from the surgery facility, always with an ASPAN score of 10.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree