Chapter 11 The Inframammary Approach for Augmentation
The inframammary approach is the most logical approach for breast augmentation if a surgeon prioritizes tissue trauma, bleeding, and accurate pocket dissection. Using the inframammary approach, a surgeon can gain access to the prosthetic pocket with minimal trauma to tissues between the incision and the pocket. Reducing tissue trauma reduces postoperative inflammation and pain, and facilitates a faster recovery with fewer potential wound healing tradeoffs. In most cases, the surgeon traverses less than 2 cm of normal tissue prior to entering the implant pocket, whether the pocket is submammary, subpectoral, or dual plane. Through the inframammary incision, all areas of the pocket are accessible to the surgeon under direct vision, allowing the highest level of control during dissection, and the most accurate pocket dimensions. Wide, direct visualization allows the surgeon to identify and control potential bleeding before it occurs (prospective hemostasis), preventing tissue staining from bleeding that occurs with conventional sharp or blunt dissection techniques that create bleeding that the surgeon must then control. Avoiding any traces of blood in tissues reduces postoperative inflammation and discomfort that prolong patient recovery and return to normal activities, and reduces risks of capsular contracture postoperatively. The inframammary approach requires very few instruments, increases efficiency and reduces operating times and doses of anesthetic medications that can unnecessarily prolong and complicate recovery.
Instrumentation for the Inframammary Approach
Optimal instrumentation is essential to reduce tissue trauma, increase efficiency, and execute the details of surgical technique that enable surgeons to deliver 24 hour recovery.1,2 Minimizing total numbers of instruments optimizes efficiency and cost effectiveness. By consolidating and optimizing the instrument set, the surgeon can increase accuracy and control, save valuable time, and reduce morbidity.
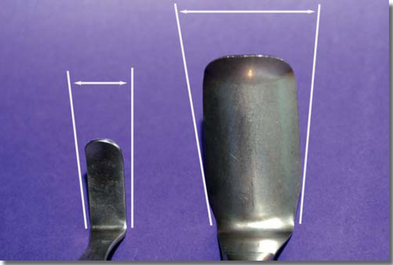
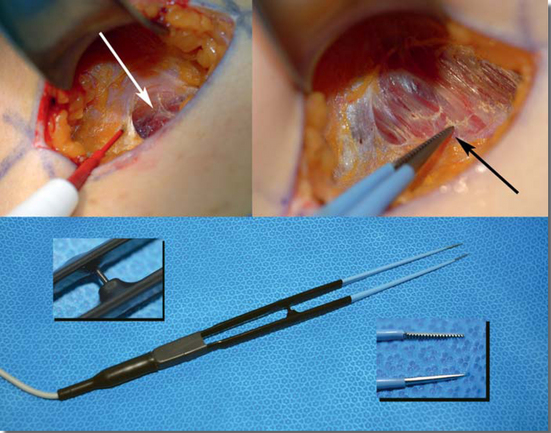
Specific instrument design features effectively reduce tissue trauma. Integrating instrument design features with specific surgical techniques improves outcomes.1,2 For example, the ratio of retractor width to retractor length is critical to optimize exposure. Choosing narrower blade retractors in order to minimize incision length is shortsighted, because a narrower retractor blade substantially reduces exposure and peripheral visibility in the pocket, increasing risks of inadvertent bleeding if the surgeon is unable to identify larger perforating vessels before dividing them (Figure 11-1, A). Retractor blades that curve slightly downward at the lateral edges of the retractor minimize skin edge and deeper tissue trauma (Figure 11-1, B), and incorporating a smoke evacuation tube into retractor design minimizes smoke in the pocket during electrocautery dissection (Figure 11-1, C), improving visualization and accuracy. Substituting a headlight and eliminating the fiberoptic bundle on retractors (Figure 11-1, D) decreases risks of the bundle contacting periosteum and causing bleeding during retractor insertion and repositioning.

Figure 11-1B A downward curvature of retractor blades can help minimize trauma to skin edges and adjacent tissues.
Minimizing retraction forces minimizes tissue trauma and bleeding. Surgeons can minimize tissue trauma and increase efficiency by following simple principles of retraction:
The Tebbetts™ breast set (Figure 11-4) includes the following instruments that are designed specifically to optimize efficiency and control when using the inframammary approach to augmentation:
The double ended retractor (Figure 11-5) is designed for multiple purposes, and is an important instrument for use with all incision approaches. The shorter blade of the retractor facilitates exposure and minimizes tissue trauma during initial stages of pocket dissection, while the longer blade provides optimal exposure as dissection proceeds more distal to the incision. By using two double ended retractors, the surgeon can insert the longer blade of a second retractor beneath the shorter blade of a retractor already in the pocket, then remove the shorter blade of the first retractor. This maneuver is far more efficient compared to completely removing, rotating, and reinserting a single retractor, reducing risks of the retractor contacting rib periosteum or perichondrium, saving time, and reducing tissue trauma and potential contamination.
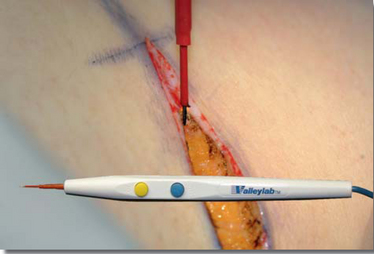
A standard scalpel incises the epidermis and superficial dermis, but avoids midlevel dermis to avoid excessive bleeding from the subdermal plexus. A needle tip electrocautery pencil with blended cut and coagulation current is ideal for incising through dermis (Figure 11-6), subcutaneous tissue, and for subpectoral and dual plane pocket locations, through pectoralis fascia. When the pectoralis muscle (or in the case of a retromammary pocket, the pectoralis fascia) becomes visible, the surgeon switches to the handswitching, monopolar, needlepoint electrocautery forceps (Figure 11-7), and performs the entire pocket development using only this one instrument for both dissection and hemostasis. Handswitching, monopolar, needlepoint electrocautery forceps have revolutionized pocket dissection for augmentation, allowing surgeons to routinely develop the entire pocket for the implant with a single instrument, in less than 5 minutes, with virtually zero bleeding and minimal residual blood in tissues.
The spatula retractor (Figure 11-8) is a specialized, multifunctional instrument that is indispensable in inframammary augmentation and in open capsulectomy, especially when used in combination with a double ended retractor. Avoiding excessive lateral pocket dissection is critically important to avoid lateral implant displacement and widening of the intermammary distance. The most predictable method to avoid excessive lateral pocket development is for the surgeon to stop lateral dissection at the lateral border of the pectoralis minor muscle initially, insert the implant, and then incrementally enlarge the lateral pocket in 0.5 cm increments until the footprint of the implant lies flat and just fits the base of the pocket. After inserting the implant, the surgeon uses a double ended retractor to retract the lateral soft tissues laterally, and a spatula retractor to retract and protect the implant medially, then enlarges the pocket incrementally using the handswitching, monopolar, electrocautery forceps.
Surgical Techniques for the Inframammary Approach
Specific details of surgical technique enable surgeons to predictably assure over 90% of patients that they can return to full, normal, non-aerobic activities within 24 hours following either subpectoral or submammary augmentation for the first time in the history of breast augmentation.1,2 This rapid recovery is remarkable, because it completely redefines the patient experience in modern augmentation mammaplasty, and is predictable using inframammary, periareolar, and axillary incision approaches. Rapid recovery and return to normal activities within 24 hours is impossible without dramatically reducing tissue trauma and bleeding. The following techniques, combined with optimal anesthetic management, predictably allow surgeons to deliver their patients a completely redefined experience in breast augmentation.
Table 11-1 is a detailed script in tabular form that details surgeon and personnel subroutines for inframammary augmentation. This document details every step and every action for every person in the operating room, and derives from hundreds of hours of detailed videotape analysis, applying principles of motion and time studies.1,2 Due to the length of this document, it is included in the Resources folder on the DVDs that accompany this book.
Principles of Prospective Hemostasis
Incision Location and Length
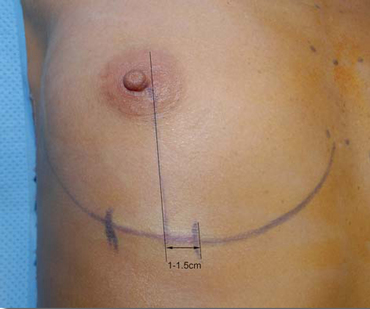
In patients with an established, well defined inframammary fold, the surgeon should place the incision in the deepest visual portion of the fold. In patients with poorly defined folds, or measured dimensions mandate lowering the fold onto chest skin, the surgeon should drop a perpendicular line from the medial border of the nipple to the inframammary fold, and then place 1–1.5 cm of the incision medial to the perpendicular line at the desired new fold level and the remainder lateral to the line (Figure 11-10).
Initial Incision and Dissection
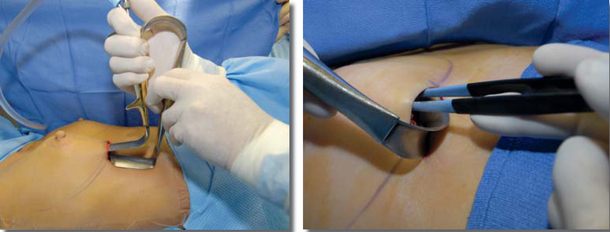
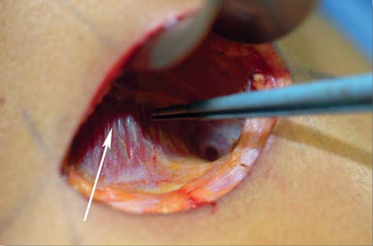
The surgeon incises skin with the scalpel according to preoperative markings, and then lifts the tissues superior to the incision with the non-dominant hand to delineate the deep subcutaneous fascia and lift it away from the underlying fascia, reducing risks of inadvertently dissecting too deeply. Switching to the handswitching needlepoint electrocautery pencil, the surgeon dissects through subcutaneous tissue and deep subcutaneous fascia to expose pectoralis fascia (Figure 11-7, top left). For a retromammary pocket, the plane of dissection remains superficial to the pectoralis fascia. For subpectoral or dual plane pocket dissection, the surgeon incises the pectoralis fascia with the electrocautery pencil, and then switches to the handswitching, monopolar, needlepoint electrocautery forceps (Figure 11-7).
Chapter 9 detailed the relative advantages and tradeoffs of retromammary, subfascial, traditional partial retropectoral, and dual plane pocket techniques. Assuring adequate soft tissue coverage long-term is the highest priority in breast augmentation, because inadequate soft tissue coverage dramatically increases risks of complications and reoperations long-term. The development of the dual plane pocket for augmentation has largely eliminated the tradeoffs of traditional subpectoral pocket locations, and if pocket location is based on logic, the dual plane pocket has rendered submammary and subfascial pockets largely obsolete. The description of technical details of inframammary augmentation in this chapter details dual plane techniques.3
Entering the Subpectoral Space
Surgeons can avoid inadvertently dissecting through the intercostal or serratus muscles, potentially causing a pneumothorax by following a simple, straightforward technique. Inserting the shorter blade of a double ended retractor with the tip at the level of the pectoralis fascia, the surgeon lifts directly anteriorly. If the underlying muscle layer tents upward (Figure 11-11), the muscle is pectoralis major. Intercostal or serratus muscles will never tent upward. After assuring that the muscle layer tents, the surgeon checks topographical landmarks, and then aims dissection medial to the areola, in the area of the subpectoral pocket where the pectoralis is never adherent to either the serratus or pectoralis minor muscles (Figure 11-12).
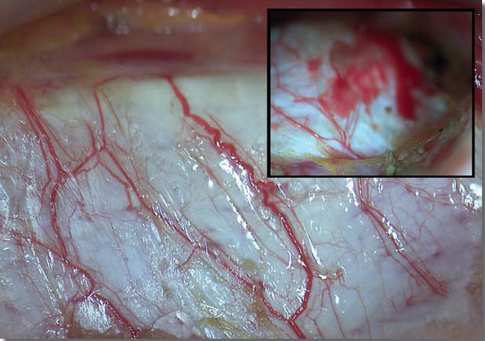
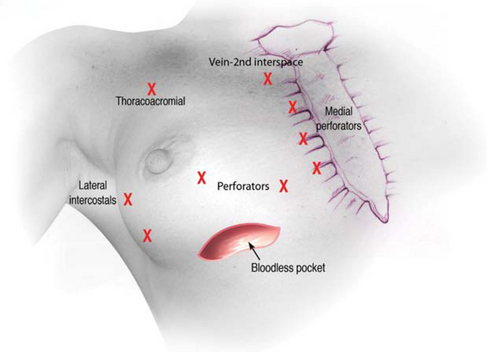
To enter the subpectoral space, the surgeon sweeps the closed needle tips of the handswitching, monopolar, electrocautery forceps back and forth over the tented pectoralis muscle, using a light, sweeping motion and dividing the pectoralis muscle at least 0.5 cm above the origins on the ribs. If the surgeon divides pectoralis origins immediately adjacent to the origin on the ribs, perforating vessels can retract and become very difficult to control without risking pneumothorax. Leaving small stumps of muscle origins on the ribs completely avoids this potential problem. Throughout this portion of the dissection, the surgeon maintains exposure using the short blade of the double ended retractor, repositioning it frequently to the most distal area of dissection to optimally define the dissection plane. As the surgeon dissects through the pectoralis origins to enter the pocket, a large perforator is usually located inferomedial to the areola (Figure 11-13). Thorough electrocoagulation with the forceps in two or three locations along the vessels before dividing them minimizes risks of bleeding from the cut stumps later in the procedure or postoperatively.
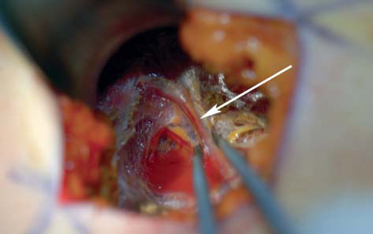
Figure 11-13 Large perforator artery and vein (white arrow), usually located inferomedial to the areola.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree