Procedure 11 Endoscopic Carpal Tunnel Release
Indications
 Failure of conservative treatment for idiopathic carpal tunnel syndrome (CTS).
Failure of conservative treatment for idiopathic carpal tunnel syndrome (CTS).
 Patient prefers the endoscopic procedure.
Patient prefers the endoscopic procedure.
 The authors’ preferred technique is the limited incision open carpal tunnel release (LOCTR) (see Procedure 12). Studies have not demonstrated significant differences in outcomes between endoscopic carpal tunnel release (ECTR) and LOCTR. ECTR has a steep learning curve, needs a sizeable initial capital investment in video equipment, and incurs the recurring cost of the single-use disposable blade. Although the time taken to perform ECTR is less than for LOCTR, the time expended to set up the equipment mitigates this advantage.
The authors’ preferred technique is the limited incision open carpal tunnel release (LOCTR) (see Procedure 12). Studies have not demonstrated significant differences in outcomes between endoscopic carpal tunnel release (ECTR) and LOCTR. ECTR has a steep learning curve, needs a sizeable initial capital investment in video equipment, and incurs the recurring cost of the single-use disposable blade. Although the time taken to perform ECTR is less than for LOCTR, the time expended to set up the equipment mitigates this advantage.
 Occasionally, patients request the endoscopic procedure. They are counseled with regard to the cost and complications. We prefer the single-portal Agee technique to the double-portal Chow technique because the Agee technique avoids a scar in the palm.
Occasionally, patients request the endoscopic procedure. They are counseled with regard to the cost and complications. We prefer the single-portal Agee technique to the double-portal Chow technique because the Agee technique avoids a scar in the palm.
Surgical Anatomy
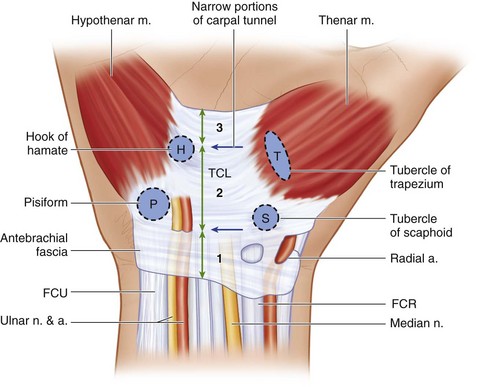
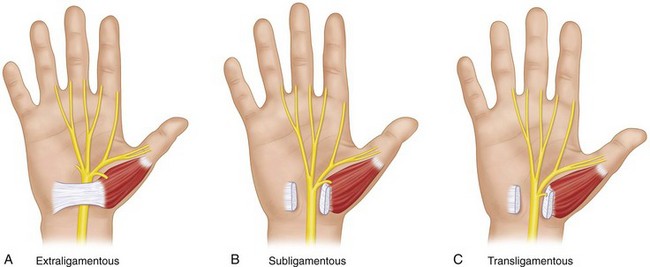
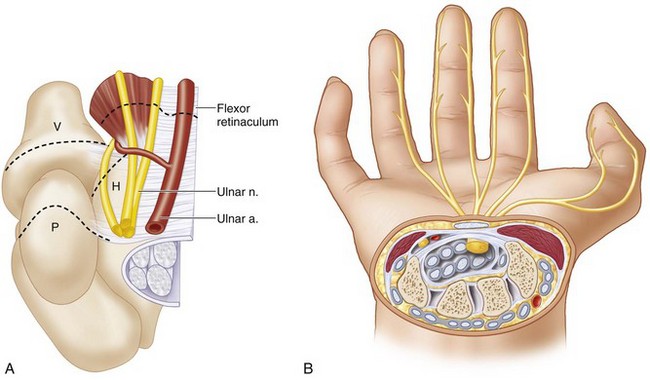
 The carpal tunnel is a fibro-osseous tunnel that contains the median nerve and the nine flexor tendons to the thumb and the fingers. The roof of the carpal tunnel is formed by the flexor retinaculum, which extends between four bony prominences (proximally: pisiform and tubercle of scaphoid, distally: hook of the hamate and tubercle of trapezium) (Fig. 11-1).
The carpal tunnel is a fibro-osseous tunnel that contains the median nerve and the nine flexor tendons to the thumb and the fingers. The roof of the carpal tunnel is formed by the flexor retinaculum, which extends between four bony prominences (proximally: pisiform and tubercle of scaphoid, distally: hook of the hamate and tubercle of trapezium) (Fig. 11-1).
 The flexor retinaculum can be divided into three components (see Fig. 11-1).
The flexor retinaculum can be divided into three components (see Fig. 11-1).
 Some authors consider the flexor retinaculum and the TCL to be synonymous.
Some authors consider the flexor retinaculum and the TCL to be synonymous.
 The carpal tunnel is narrowest in both palmar-dorsal and ulnar-radial planes at the level of the hook of the hamate. The other narrow portion of the carpal tunnel is at the proximal edge of the TCL (see Fig. 11-1).
The carpal tunnel is narrowest in both palmar-dorsal and ulnar-radial planes at the level of the hook of the hamate. The other narrow portion of the carpal tunnel is at the proximal edge of the TCL (see Fig. 11-1).
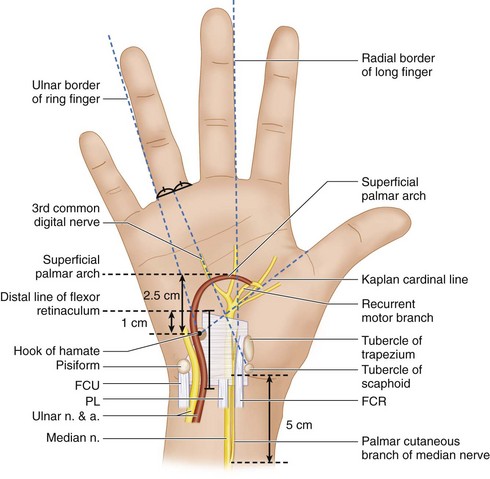
 The important surface landmarks and surrounding neurovascular structures related to the carpal tunnel are as follows (Fig. 11-2):
The important surface landmarks and surrounding neurovascular structures related to the carpal tunnel are as follows (Fig. 11-2):
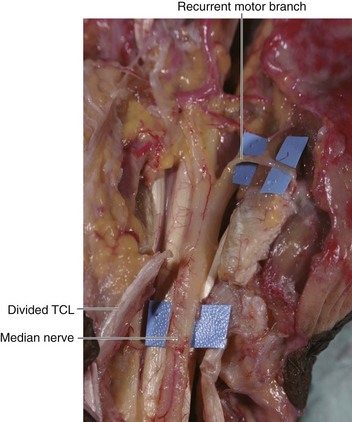
 The ulnar nerve and artery overlie the ulnar border of the flexor retinaculum and may be at risk during ECTR. The nerve is generally anterior or ulnar to the hook of the hamate, but the artery is often immediately superficial to the flexor retinaculum lying within a fat-filled space (Fig. 11-5).
The ulnar nerve and artery overlie the ulnar border of the flexor retinaculum and may be at risk during ECTR. The nerve is generally anterior or ulnar to the hook of the hamate, but the artery is often immediately superficial to the flexor retinaculum lying within a fat-filled space (Fig. 11-5).
Positioning
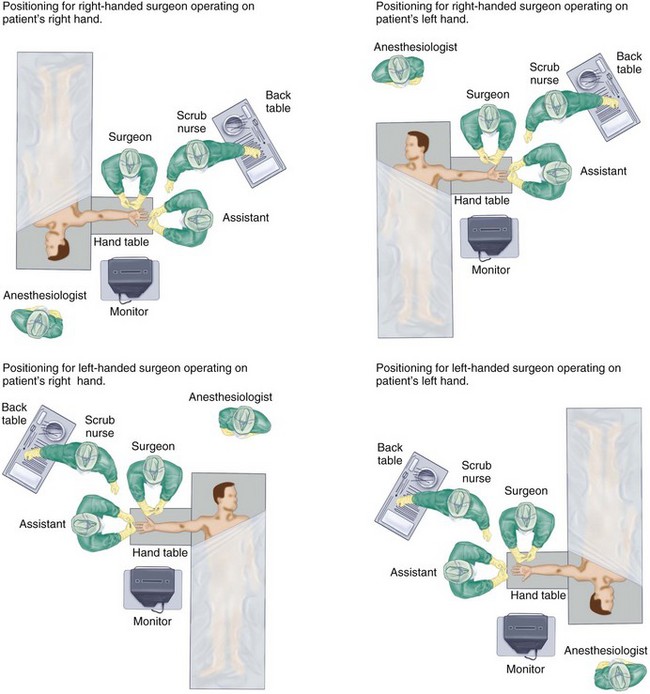
 The procedure is performed under tourniquet control with the patient in supine position and the affected extremity on a hand table. The positioning of surgeon, patient, and anesthesiologist is shown in Figure 11-6.
The procedure is performed under tourniquet control with the patient in supine position and the affected extremity on a hand table. The positioning of surgeon, patient, and anesthesiologist is shown in Figure 11-6.
 It can be done under general regional anesthesia, intravenous regional (Bier block) anesthesia, or local anesthesia.
It can be done under general regional anesthesia, intravenous regional (Bier block) anesthesia, or local anesthesia.