Chapter 10 Surgical Principles and Instrumentation
Specific surgical principles are critical to optimize the patient experience and outcomes in breast augmentation, regardless of the incision approach, pocket location, or type of implant. Compulsively addressing seemingly minor technical issues can dramatically impact the patient experience, outcomes, and reoperation rates. Analyzing every aspect of surgical technique and continually improving efficiency and eliminating unnecessary and unproductive actions using process engineering principles1,2 can dramatically impact short- and long-term outcomes. Optimally controlling surgical variables that impact outcomes requires that surgeons continually reassess established practices, avoid preconceptions, and demonstrate a willingness to implement proved processes.1–4
Impact of Decision Processes and Surgical Planning
Chapter 7 details principles and methodologies that optimize surgical planning. Surgical planning and the decision process define and limit the potential success of every surgical maneuver. Every suboptimal or unnecessary surgical maneuver increases bleeding and tissue trauma, increases operative time and costs, increases medication doses intraoperatively, decreases the predictability of the outcome, and increases risks of complications and reoperations. The key for surgeons is to identify and optimize surgical maneuvers that are proved to impact outcomes, and eliminate all maneuvers, techniques, and adjuncts that are unnecessary and unproductive.
Currently available systems and decision processes for preoperative implant selection3,5 eliminate any need for sizer implants in routine primary augmentation, and reduce or eliminate the costly practice of surgeons ordering multiple sizes of implants for every breast augmentation
Some of the most inefficient, time wasting practices intraoperatively relate to implant selection and the use of intraoperative sizer implants. Currently available systems and decision processes for preoperative implant selection3,5 eliminate any need for sizer implants in routine primary augmentation, and reduce or eliminate the costly practice of surgeons ordering multiple sizes of implants for every breast augmentation. In addition to unnecessarily increasing operative times and costs, routine use of sizer implants increases risks of pocket contamination, may increase tissue trauma and bleeding, and has no proved necessity or efficacy in valid scientific studies.
Operative planning is most productive and least prone to errors of omission when surgeons complete defined forms3,5 that record objective measurement data and record decisions and operative plans, and then have these forms available in the operating room for every breast augmentation. Having standardized, preoperative photographs in the operating room is also helpful, but virtually every decision that a surgeon makes looking at photographs in the operating room could have been made preoperatively and recorded on the operative planning form, increasing efficiency and accuracy.
Direct Vision Access and Pocket Dissection Techniques
Blunt and blind (no direct vision inside the pocket) dissection techniques unquestionably increase tissue trauma and bleeding and decrease the accuracy of pocket dissection compared to techniques that perform pocket dissection under direct vision, with or without endoscopic assistance. While blunt dissection and blunt, blind dissection techniques remain in common use, no peer reviewed and published studies and no live surgery demonstrations have ever documented equivalent patient recovery and outcomes compared to more controlled, accurate, and efficient direct vision techniques.1,2,6,7
Inframammary and periareolar incision approaches allow surgeons to perform all areas of pocket dissection under direct vision control, but some surgeons continue to use digital or blunt instrument dissection techniques, citing the speed and efficiency of blunt dissection techniques. In reality, blunt dissection techniques cannot compare with optimal electrocautery dissection techniques with respect to efficiency, because the former produces bleeding which the surgeon must control, while the latter prevents bleeding before it occurs and routinely allows surgeons to develop an entire pocket via the inframammary approach in less than 4 minutes.2,4,7 The author’s experience with blunt dissection for axillary augmentation8 and subsequent experience with optimal electrocautery dissection techniques2,9 has produced conclusive evidence that blunt dissection techniques are more inefficient, prolong operating times, and significantly increase morbidity and prolong recovery compared to direct vision, electrocautery techniques.
Current endoscopic instrumentation enables surgeons to perform all areas of pocket dissection in axillary augmentation under direct vision control. For optimal recovery and outcomes, surgeons should avoid any blunt dissection whatever in axillary augmentation, and use optimal endoscopic instrumentation9 to optimize control, minimize tissue trauma, and minimize bleeding.
For optimal recovery and outcomes, surgeons should avoid any blunt dissection whatever in axillary augmentation, and use optimal endoscopic instrumentation9 to optimize control, minimize tissue trauma, and minimize bleeding
Despite claims by its proponents that the umbilical approach for augmentation provides equivalent outcomes to direct vision approaches, current descriptions of surgical techniques for the umbilical approach do not allow surgeons direct vision control inside the pocket during pocket dissection. Dissection techniques are blunt and blind, and recovery data are not equivalent to techniques that use direct vision techniques.2,7,9
Incision Length
With state-of-the-art form stable, silicone gel implants such as the Allergan Style 410, incision lengths should be longer to facilitate exposure and implant insertion while avoiding damage to the implant. Implant dimensions and volume determine optimal decisions of incision length for form stable implants. When planning incision length for the form stable Allergan Style 410, to minimize risks of device damage and reoperations,4 surgeons should plan a minimum incision length of 5.0–5.5 cm for Style 410 implants less than 300 grams, and 6.0–6.5 cm for implants larger than 300 grams. These guidelines afforded a level of patient satisfaction and device safety that defined a zero percent reoperation rate in a consecutive premarket approval (PMA) series.
Surgical Instrumentation
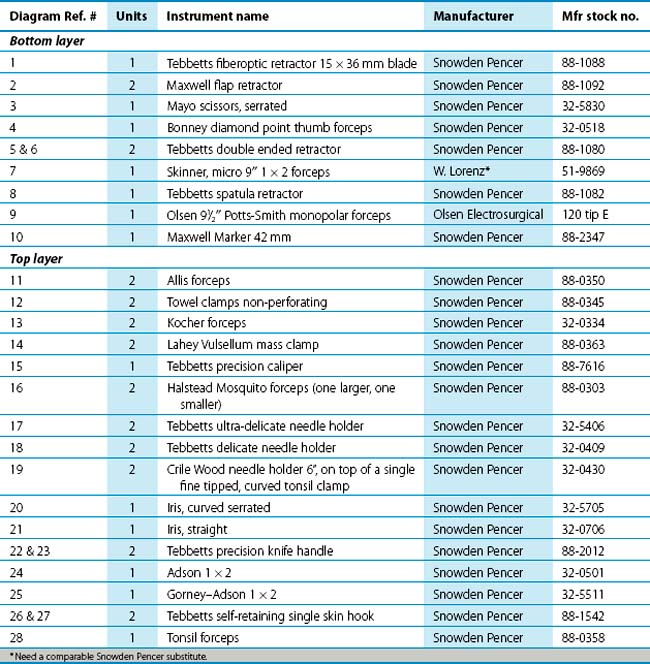
 Inframammary and periareolar approaches for breast augmentation are optimized by specific instrumentation that can improve efficiency and accuracy while decreasing tissue trauma. The author’s breast instrument set (Figure 10-1) includes instruments for augmentation and all other types of breast surgery. Instruments in the set are listed in Table 10-1. Instruments in the set are designed or modified from other designs to optimize efficiency and accuracy. A limited number of these instruments are required to perform augmentation via the three main incision approaches, and the specific use of each instrument is detailed in respective chapters that address each incision approach.
Inframammary and periareolar approaches for breast augmentation are optimized by specific instrumentation that can improve efficiency and accuracy while decreasing tissue trauma. The author’s breast instrument set (Figure 10-1) includes instruments for augmentation and all other types of breast surgery. Instruments in the set are listed in Table 10-1. Instruments in the set are designed or modified from other designs to optimize efficiency and accuracy. A limited number of these instruments are required to perform augmentation via the three main incision approaches, and the specific use of each instrument is detailed in respective chapters that address each incision approach.
Specialized instrumentation for axillary augmentation includes a right angled endoscope that moves the endoscope camera away from the single access port for the operation and a specialized, multipurpose electrocautery dissection instrument that are described in detail inChapter 12.
Retractor design and specific techniques for positioning and repositioning retractors optimize exposure and minimize tissue trauma. The narrower a retractor blade, the narrower the surgeon’s field of vision at the most distal extent of the surgical exposure area. Optimal retractor widths for inframammary, periareolar, and the upper pocket in axillary augmentation are at least 2.5–3 cm. Retractors narrower than 2.5 cm limit exposure. While surgeons can successfully perform augmentation with narrower retractors, during dissection the surgeon cannot visualize areas of the pocket adjacent to the immediate area of dissection as clearly, and surgeons are less likely to identify and control blood vessels before cutting them. This seemingly minor issue of retractor width can make a substantial difference in the accuracy and efficiency of pocket dissection.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree