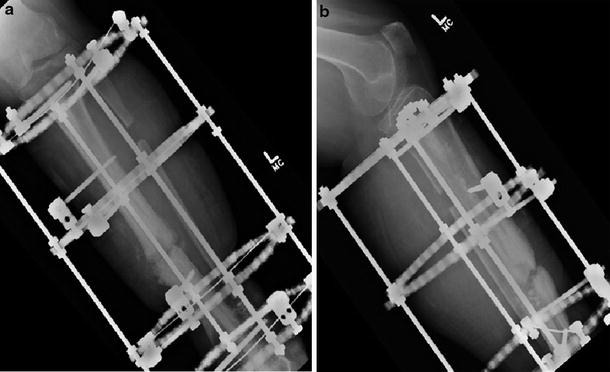
Fig. 1
(a) Lateral and (b) AP: history of TTC nail for prior trauma and tibial nonunion. Note prior ankle fusion

Fig. 2
(a) AP and (b) lateral s/p hardware removal and cultures
3 Preoperative Problem List
Leg pain
Gait dysfunction/inability to ambulate
Infected nonunion left tibia
Penicillin allergy
Elevated CRP
S/p ankle (pantalar) arthrodesis
4 Treatment Strategy
The patient initially demonstrated an infected hypertrophic nonunion, with a combination of instability due to fracture in a high-stress area (above ankle fusion) and infection inhibiting healing. Addressing both aspects of this failure would be required to achieve healing. Thorough debridement, requiring three separate significant surgical debridement procedures, was employed to remove infectious bio-burden . Placement of depot antibiotics in a resorbable (CaSO4) carrier provided high local concentration and avoided the need for yet another procedure to remove a nonabsorbable delivery system. Throughout this, the fracture site was stabilized firmly with compression using a stable, adjustable strut fixator. We utilized both fine wires to minimize tissue irritation and half pins maximize bony stability. Due to the patient’s long history of infection, and changing microbial culture results, several rounds of IV and oral antibiotics were employed. Ambulation helped the patient remain functional and also provided physiologic loading to stimulate fracture healing.
5 Basic Principles
Treatment of osteomyelitis using the principles of the Cierny-Mader staging system applies to infected nonunion of the bone as in this case. This patient was initially a “B” host, with locally compromised tissues due to infection and fracture instability, with stage 4 (diffuse/nonunion) anatomy. Meticulous irrigation with normal saline, and debridement to the healthy bleeding bone, (visualizing the “paprika sign”) with rongeurs, burrs, and high-speed bone surgical drill (Midas Rex Acorn bit 8AC60-MN), followed by placement of local antibiotic depot treatment of the fracture, downstages the disease to stage 4A. Systemic antibiotic treatment and stabilization with fixator improves the patient’s global health and local tissues and her ambulatory function, making her an “A” host. External fixation stabilizes the bone so both antibiotic treatment of the infection and bone healing are able to proceed.
Fixation of the nonunion/fracture follows AO principles, with the initial hypertrophic nonunion requiring increased stability, in this case frame compression, producing compression at the fracture/nonunion site, for bone healing.