Procedure 10 Extensor Tendon Repair in Zones 1 to 5
![]() See Video 7: Turnover Tendon Flap for PIP Extensor Tendon Injury
See Video 7: Turnover Tendon Flap for PIP Extensor Tendon Injury
Surgical Anatomy
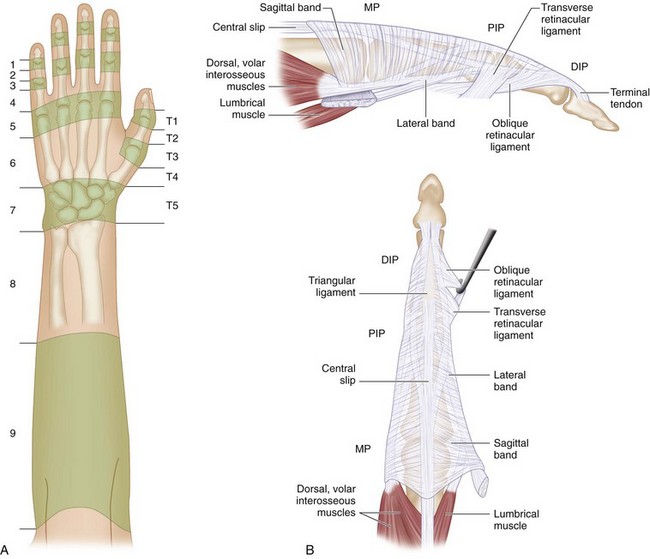
 Extensor tendon injuries are divided into nine zones for the fingers and seven zones for the thumb numbered from distal to proximal (Fig. 10-2A). An easy way to remember these zones is to bear in mind that the odd-numbered zones are located over the joints. Therefore zones 1, 3, 5, and 7 are located over the distal interphalangeal (DIP) joint, proximal interphalangeal (PIP) joint, metacarpophalangeal (MCP) joint, and wrist, respectively.
Extensor tendon injuries are divided into nine zones for the fingers and seven zones for the thumb numbered from distal to proximal (Fig. 10-2A). An easy way to remember these zones is to bear in mind that the odd-numbered zones are located over the joints. Therefore zones 1, 3, 5, and 7 are located over the distal interphalangeal (DIP) joint, proximal interphalangeal (PIP) joint, metacarpophalangeal (MCP) joint, and wrist, respectively.
 The extensor tendon is thick over the MCP joint but becomes broad and thin over the dorsum of the proximal phalanx, where it divides into three portions. The central portion becomes the central slip that inserts into the base of the middle phalanx, and the lateral portions join the lateral bands. The tendons of the lumbrical and interosseous muscles form the lateral bands. These lateral bands come together over the middle phalanx and form the most distal part of the extensor tendon that inserts into the base of the distal phalanx (Fig. 10-2B).
The extensor tendon is thick over the MCP joint but becomes broad and thin over the dorsum of the proximal phalanx, where it divides into three portions. The central portion becomes the central slip that inserts into the base of the middle phalanx, and the lateral portions join the lateral bands. The tendons of the lumbrical and interosseous muscles form the lateral bands. These lateral bands come together over the middle phalanx and form the most distal part of the extensor tendon that inserts into the base of the distal phalanx (Fig. 10-2B).
 At the MCP joint, the extensor tendon is held in position by the sagittal bands, which arise from the volar plate of the MCP joint and the intermetacarpal ligaments, to insert on the extensor hood. Injury to the sagittal bands may result in subluxation of the extensor tendon.
At the MCP joint, the extensor tendon is held in position by the sagittal bands, which arise from the volar plate of the MCP joint and the intermetacarpal ligaments, to insert on the extensor hood. Injury to the sagittal bands may result in subluxation of the extensor tendon.
 There is very little excursion of the extensor tendon over the fingers (11 to 17 mm at the MCP joint, 6 to 8 mm at the PIP joint, and 4 to 5 mm at the DIP joint). It is therefore important to do an accurate repair and avoid bunching up the tendon. It is usually possible to pass a core suture through the extensor tendon in the proximal half of zone 4 and in zone 5. However, only a simple suture is possible in zones 1, 2, and 3.
There is very little excursion of the extensor tendon over the fingers (11 to 17 mm at the MCP joint, 6 to 8 mm at the PIP joint, and 4 to 5 mm at the DIP joint). It is therefore important to do an accurate repair and avoid bunching up the tendon. It is usually possible to pass a core suture through the extensor tendon in the proximal half of zone 4 and in zone 5. However, only a simple suture is possible in zones 1, 2, and 3.
 Lacerations to the extensor pollicis longus (EPL) tendon cannot be tested by simply examining extension of the thumb interphalangeal (IP) joint. The IP joint may be extended by the extensor pollicis brevis (EPB) and the thenar intrinsic muscles via their insertions on the extensor expansion. The EPL is tested by placing the patient’s hand flat on a table and asking the patient to lift the thumb off the table (Fig. 10-3).
Lacerations to the extensor pollicis longus (EPL) tendon cannot be tested by simply examining extension of the thumb interphalangeal (IP) joint. The IP joint may be extended by the extensor pollicis brevis (EPB) and the thenar intrinsic muscles via their insertions on the extensor expansion. The EPL is tested by placing the patient’s hand flat on a table and asking the patient to lift the thumb off the table (Fig. 10-3).
Positioning
 Extensor tendon repairs can be done under a digital block (zones 1, 2, and 3) or a wrist block (zones 4 and 5). The use of a forearm tourniquet (placed distally over the nonmuscular portion of the forearm) will allow the patient to tolerate the tourniquet for a longer period (30 to 40 minutes) compared with the usual placement over the arm (20 to 30 minutes). The patient is positioned supine with the affected extremity on a hand table.
Extensor tendon repairs can be done under a digital block (zones 1, 2, and 3) or a wrist block (zones 4 and 5). The use of a forearm tourniquet (placed distally over the nonmuscular portion of the forearm) will allow the patient to tolerate the tourniquet for a longer period (30 to 40 minutes) compared with the usual placement over the arm (20 to 30 minutes). The patient is positioned supine with the affected extremity on a hand table.
Exposures
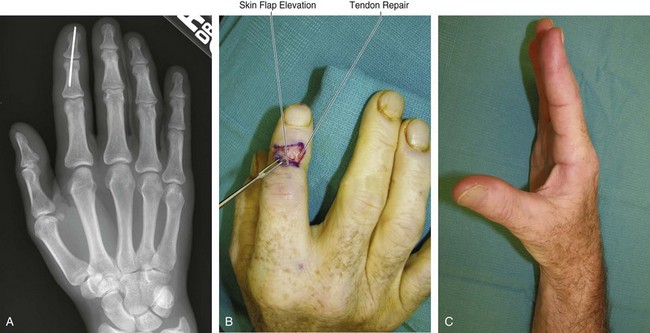
 The existing lacerations are incorporated to raise wide flaps with a broad tip.
The existing lacerations are incorporated to raise wide flaps with a broad tip.
 Full-thickness skin flaps are raised superficial to the paratenon.
Full-thickness skin flaps are raised superficial to the paratenon.
Zone 1 Injury
Clinical Examination
 Patients present with a flexed posture of the DIP joint (mallet finger) and inability to actively extend the DIP joint (Fig. 10-4).
Patients present with a flexed posture of the DIP joint (mallet finger) and inability to actively extend the DIP joint (Fig. 10-4).
 Patients with an untreated mallet finger, especially those with a preexisting hyperextensible PIP joint, can develop a compensatory swan-neck deformity because of extensor force being directed toward the central slip and leading to hyperextension at the PIP joint.
Patients with an untreated mallet finger, especially those with a preexisting hyperextensible PIP joint, can develop a compensatory swan-neck deformity because of extensor force being directed toward the central slip and leading to hyperextension at the PIP joint.
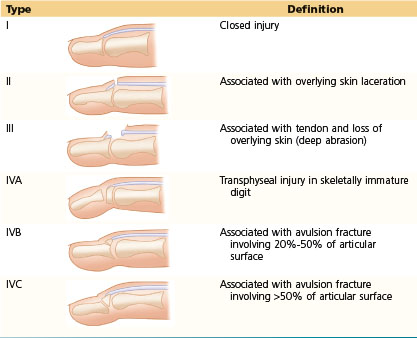
 Doyle has classified mallet finger into four types (Table 10-1).
Doyle has classified mallet finger into four types (Table 10-1).
Table 10-1 Classification of Mallet Finger